
nhs ribbon being cut alamy suo 3×2
There have been rationing drives before – but never one like this. Last month, a CCG was on the verge of the unthinkable: putting a ban on all non-urgent GP referrals this winter.
The proposal was enough to stun even hardened cynics – although eventually NHS St Helens CCG was forced to back down on its plan to freeze outpatient referrals until March 2017 amid widespread condemnation from GPs and others. However, the St Helens situation was just the latest symptom of a system struggling to cope.
NHS England figures reveal that 39 CCGs ended the last financial year with deficits that totalled an eye-watering £700m.
But this was nothing compared with the deficits in hospital trusts, which have required an extra £1.8bn from NHS England just to cut the shortfall to £250m.
Even NHS England chief executive Simon Stevens admitted last month that ‘individual hospitals were choosing their deficit and then expecting someone else to pick up the tab’.
Pulse warned GPs last August that a gaping ‘black hole’ in the NHS finances would mean a renewed rationing drive in primary care, and this is now starting to occur.
St Helens is one of the 26 CCGs across England rated ‘inadequate’ by NHS England, largely due to financial difficulties.
Its plan to halt all GPs referrals for non-urgent interventions such as hip operations and cataract surgery over the busy winter period was part of a ‘financial recovery’ plan to tackle a £12.5m funding gap. The Merseyside CCG acknowledged the idea would be ‘unpopular’, but said that ‘activity in the hospital exceeds the budget we receive’.
Unacceptable
But it later withdrew the proposal completely after it hit the national media headlines. At the time, GPC deputy chair Dr Richard Vautrey said it was an ‘unacceptable decision’: ‘The cost to the health service of delaying referrals could ultimately be much greater in the long term as more complex and costly problems develop as a result.’
But St Helens is not alone. NHS Northern, Eastern and Western Devon CCG is another ‘inadequate’ CCG that is having to think the unthinkable.
How about the devolved nations?
In the devolved nations, GPs report things are not as bad as in England, but there are concerning signs.
In Scotland, health boards need to make combined savings of £40m this year. Dr Andrew Buist, deputy chair of Scottish GPC, says there are ‘longer waiting lists and more protocols’, such as trusts only seeing patients if they’ve had ‘certain tests, X-rays, meet criteria or don’t have any exclusion criteria’.
Welsh GPC chair Dr Charlotte Jones says there has been nothing like refusing referrals, but ‘as things get tighter, we are concerned it will be more of a problem’. She cites the example of health boards being less willing to commission treatment in specialist centres in England.
It ended 2015/16 with a deficit of £107m and Pulse recently revealed that it was developing a controversial scheme to shift an enormous amount of hospital work onto GPs. The local LMC is furious at the scheme, which could see GP practices initially taking on the management of a third of urology referrals – with no extra funding – with plans to roll the scheme out to other hospital departments in future.
Dr Mark Sanford-Wood, medical secretary at Devon LMC, says: ‘For each of those outpatient attendances saved they could use the money to reinvest in general practice to do the work, and they aren’t doing that. It is, first and foremost, a cost-saving measure.’
NHS Basildon and Brentwood CCG has gone further than ever before in its bid to cut costs. It is proposing a stop to all bariatric surgery, after limiting vasectomy referrals last year.
These are just three of the CCGs considering drastic measures to meet their overriding statutory duty to achieve ‘financial balance’. They are faced with the threat of being disbanded or usurped by an ‘accountable care organisation’ if they fail to balance their books under NHS England’s new strategy to ‘re-set’ health service finances.
The 18-week waiting target is being deliberately allowed to slide and others are looking to trim GP prescribing and LES budgets.
Hanging on
NHS Walsall CCG and NHS Kernow CCG are currently reviewing all their local contracts with GP practices with a view to making savings.
NHS Kernow CCG says it is facing ‘a serious and challenging financial position’. Dr Beth McCarron, a former GPC negotiator and member of the Cornwall LMC executive, says this is ‘causing considerable concern’.
She says: ‘Many practices are hanging on by their fingernails and even relatively small shifts in funding away from general practice can destabilise them.’
NHS Walsall CCG says ‘no decision has yet been taken’ but medical secretary of Walsall LMC Dr Uzma Ahmad says the move in her area to cut LESs – such as those for near-patient testing and phlebotomy – has come because GPs were outperforming expectations.
Dr Ahmad says: ‘They don’t appreciate the positive impact on the hospital and patients. [The high payment] is because there is a good uptake and we are getting good results, so they are having to pay us – it is activity based.’
CCGs in financial trouble
In ‘special measures’
Coventry and Rugby, Croydon, East Surrey, Enfield, North Somerset, North Tyneside, South Gloucestershire, Vale of York, Walsall
‘Inadequate’
Bedfordshire, Brighton and Hove, Cambridgeshire and Peterborough, Coventry and Rugby, Cumbria, East Surrey, Enfield, Havering, Herefordshire, Kernow, Medway, NEW Devon, North Hampshire, North Somerset, North Tyneside, Northumberland, Shropshire, South Cheshire, South Devon and Torbay, South Gloucestershire, Southport And Formby, St Helens, Surrey Downs, Vale Of York, Walsall, West Cheshire
But experts are warning it could get worse, with grave concerns that NHS England’s new ‘Sustainability and Transformation Plans’ (STPs) will unleash further cuts to funding of GP services in order to put NHS finances back on a sustainable footing.
These plans are being delivered by ‘local health and care systems’ within each of 44 ‘geographical footprints’ across England. NHS England claims they are to ensure services are ‘built around the needs of local populations’. But little is known about them as they have been drawn up with little or no public scrutiny. Pulse recently revealed that GPs were being actively excluded from discussions related to STPs.
Birmingham LMC medical secretary Dr Robert Morley said that in his area the LMC has ‘indirectly had sight of’ proposals to do with ‘delivery at scale’ general practice but that ‘there has been no consultation on their plans’. Londonwide LMCs told Pulse that in some cases GPs were being excluded from the process altogether.
But there are suggestions STPs could cause pain to local health economies. For example, local newspapers in north-west London are reporting leaked STPs showing moves to cut 500 hospital beds and shift care into the community.
Dr Sandford-Wood says: ‘The concern nationally is STPs will simply become secondary care overspend bailout vehicles, with little or no genuine investment in primary care and will therefore fail to meet the GP Forward View.’
He adds that even the ‘very modest aim’ for general practice to receive a 14% funding uplift by 2020 ‘may actually be subverted by STPs that pump all the money into hospitals while the whole system collapses’.
The worry is that just as primary care is being prioritised for investment, it will be undermined yet again by deficits elsewhere. Plus ça change.
What CCGs are targeting

urine test alamy suo 330x330px
Referrals
NHS St Helens CCG has dropped plans to halt non-urgent referrals but there are other proposals that will affect GPs’ ability to refer.
A new NHS Northern, Eastern and Western Devon CCG scheme has seen a third of all urology referrals sent back to GPs recommending they order certain tests and follow a management plan – with no further resources. The plan is to roll this out to other specialties.
Pulse also understands Londonwide LMCs are in talks with local CCGs over an £18m ‘referral optimisation’ scheme, and NHS Basildon and Brentwood CCG is stopping all bariatric surgery.

blood test 330x330px
LESs
Pulse reported last month that CCGs had ploughed £200m into enhanced services since 2013/14. But not all practices have been so lucky, with more cash-strapped CCGs looking at cutting enhanced services.
NHS Walsall CCG and NHS Kernow CCGs are currently reviewing all their local contracts with GP practices with a view to making savings.
Dr Beth McCarron, a former GPC negotiator and a member of Cornwall LMC, says the review is ‘short-sighted and unnecessary’.

paracetamol 330x330px
Prescribing over-the-counter medicines
Pulse has reported that 12 CCGs are bringing in plans to cut prescribing of OTC medications.
Three Leicestershire CCGs are even proposing to limit long-term prescriptions of paracetamol for treatment of arthritic pain, arguing they cost £1.5m a year and patients could buy it cheaply.
But under GMC rules GPs could face complaints. GPC prescribing spokesperson Dr Andrew Green says: ‘There is the world of difference between GPs properly encouraging patients to self-care and denying them drugs that they have recommended.’

knee surgery alamy suo 330x330px
Waiting times
Official figures already show the numbers waiting longer than 18 weeks for treatment have doubled in the past year, with thousands of operations being cancelled at the last minute (see below).
GPs bear the brunt of this as patients ask them to expedite their appointment or think they have been forgotten; this is a form of ‘covert rationing’, according to GPC deputy chair Dr Richard Vautrey.
A recent ITV News investigation found one in seven hospital trusts had been forced to suspend acute services because of staff shortages.
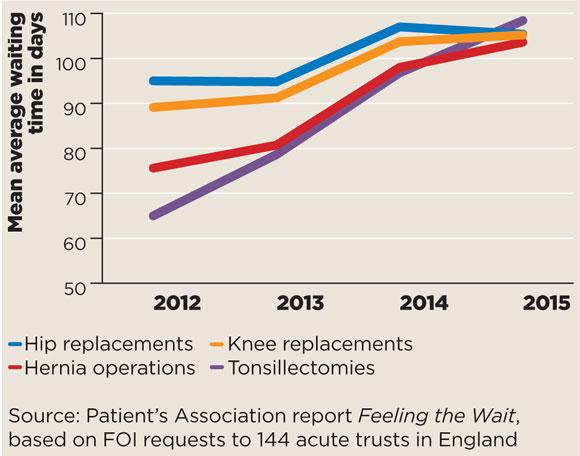
waiting times line graph 580x456px
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.












