GPs are bearing the brunt of an increase in private companies offering ‘unnecessary’ health screening tests.
A Pulse investigation has found that GPs are facing increased workloads due to a proliferation of screening tests being offered by private firms, insurers, employers, charities and ad hoc screening companies.
The body overseeing NHS screening programmes says it is worried about the way these tests are being sold – potentially causing people more harm than good – while the BMA is calling for tighter regulation.
GPs tell Pulse they are seeing patients harmed as a result, in some cases seriously – including one patient who had a kidney removed after a benign tumour came up on a private scan. But more widely, it is causing patients needless anxiety, and burdening GPs with extra, unnecessary workload.
Lack of regulation
In almost all cases the screening tests being offered – including blood tests, ECGs and even diagnostic imaging tests such as CT scans – are not recommended on the NHS, either because they are unsuitable for screening purposes or because the evidence shows they may do more harm than good.
But due to a lack of regulation, companies are offering them, with GPs often left to pick up the pieces. Glasgow GP Dr Margaret McCartney, RCGP lead on overdiagnosis and the profession’s leading campaigner against private testing, says:
‘I am concerned there is little investigation of the impact of private health screening on the NHS. There are numerous companies whose management seems to consist of handing the patient a 50-page dossier and highlighting supposedly “abnormal” results, which they are told to discuss with their GP.’
In one extreme example, a Surrey GP, who asked to remain anonymous, describes how a patient ‘following a scan, found a tumour on their kidney and was referred to the NHS; the kidney and tumour were removed, but it turned out to be benign’.
More common is the increase in unnecessary anxiety. GPC deputy chair Dr Richard Vautrey says: ‘Patients become extremely worried and may push for further investigations, which can lead to problems as well, and they are left with this constant, nagging doubt that there is something wrong with them when they are actually perfectly well.’
Many GPs are dealing with the effects of this on the ground. Around 43% of 1,170 GPs surveyed by Pulse said they had noticed an increase in workload due to private testing over the past year – compared with 50% who say they haven’t.
GPs say private screening is often regionalised, with wealthier areas predominantly affected. And private healthcare analysts LaingBuisson suggest the increase is marked, saying: ‘We estimated growth in private health screening revenues at 5% to 7% in 2014 and 2015, which was an acceleration on previous years.’
Dr Nick Summerton, a GP in East Yorkshire and medical director at health screening company Bluecrest, which offers a raft of tests through direct marketing approaches, agrees: ‘All I can say is, the growth Bluecrest has seen over the past two to three years is highly significant.’
Part of this is due to private firms adopting new sales strategies, such as selling a range of packages to middle-aged professionals as one-off services or offering workplace medicals through employee health insurance schemes.
Alongside this, there has been a rise in local screening promotions by charities, often with celebrity endorsement, while GPs are reporting an increase in UK-based patients being tested overseas.
GPC clinical and prescribing policy lead Dr Andrew Green says patients are not being given the full picture by these groups, adding that ‘very few’ men opt for PSA testing when he explains the pros and cons, yet ‘when people attend private screening they all seem to opt for it… the conclusion has to be they are not counselled properly’.
Indeed, this sort of information shortfall has led the Advertising Standards Authority to uphold five complaints about misinformation in adverts for health screening in the past five years.
And there are concerns at the highest level that this is simply ‘unethical’. Dr Anne Mackie, director of screening programmes at the UK National Screening Committee (NSC) – the body that evaluates screening tests for the Government – tells Pulse: ‘The UK NSC will only recommend screening for a condition if the benefits clearly outweigh the harms. Some of the conditions screened for by private companies are not recommended by the UK NSC and there are concerns that the potential harms of this screening are not clearly presented to the patient.’
Lifestyle
Dr Mackie adds: ‘Offering screening without explaining fully the risks relating to false positives, which can lead to raised anxiety and further unnecessary diagnostic tests, and false negatives that provide false reassurance, is unethical.’
Private companies tell Pulse they are simply offering patients the opportunity to take control of their health and make lifestyle changes.
A BUPA spokesperson says: ‘Of the patients who had lifestyle coaching after their health assessment in 2016, 80% felt their lifestyle habits had improved, 75% felt their health and wellbeing had improved, and 60% felt they were better at coping with stress.’
Meanwhile Dr Summerton says any significant findings from a Bluecrest screening session are followed up by the company’s GPs. He believes the company may have picked up ‘over 100 early bowel cancers’ over the past year through offering FIT screening tests.
But GP leaders are demanding stricter controls. Dr Vautrey says the GPC wants ‘much tighter “kite marking” or regulatory processes before private companies approach patients directly’.
Dr McCartney says she is in ‘informal talks’ with the House of Commons Health Committee about potential solutions, including a levy on private companies to pay the NHS for the work they create through tests the health service does not recommend. But she concludes: ‘We need some sort of legislation to underscore the principle that these tests are not evidence-based – perhaps an “anti-quackery” clause that customers must sign before consenting to screening.’
PSA tests
c0306166 psa test requisition spl 330x330px
The UK National Screening Committee last year again ruled out prostate cancer screening because the PSA test is too unreliable, and the harms of treating men who incorrectly test positive outweigh the benefits.
But private companies routinely include PSA testing in their screening packages, overriding Government advice that GPs should only consider offering the test to men who present with symptoms, are considered to be high risk or who are aged 50 or over and ‘proactively’ request it.
As well as this, football clubs are now collaborating with charities to invite men to specially laid-on clinics where they have their PSA levels tested.
Dr Sumegha Pathak, a GP in Stoke-on-Trent, says: ‘Our local Lions Club offers PSA testing to all men. I have to then counsel men (who are clearly worried they have cancer due to the result) on a test I did not request and would never have requested in the men that came to me.
‘They then have to undergo a prostate examination, which they dislike and find uncomfortable, which takes up the nurse’s time as a chaperone. None of them has been diagnosed with prostate cancer to date.’
ECGs
ecg SUO
Many screening packages include an ECG – resting and sometimes during exercise – to check for ‘general heart health’ and signs of arrhythmia – principally atrial fibrillation in older people.
However, the National Screening Committee recently ruled out screening for sudden cardiac death with ECGs in young people, or screening for AF in the elderly, finding the harms would outweigh the benefits.
Staffordshire GP Dr Bindu Praveen says she recently saw a patient who had a private ‘over-40 health check’, including an ECG. She added: ‘The patient was asking for referral to cardiology… all causing unnecessary patient anxiety on an already anxious man and strain on NHS resources.’
CT/MRI scans
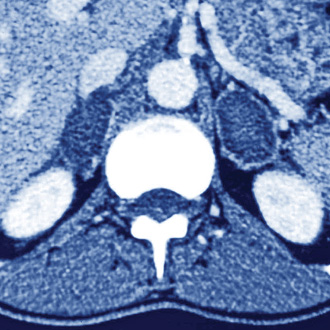
c0129675 adrenal gland tumors spl 330x330px
Some companies include advanced imaging tests in full health ‘MOTs’ – usually CT scans but, sometimes MRIs, despite these tests being intended for diagnostic purposes only.
The scans themselves come with a certain health risk because of the radiation exposure and also commonly detect ‘incidentalomas’ – benign growths that were unlikely to have caused any problem but lead to further investigations and even unnecessary interventions.
GPs also report feeling pressured into ordering such imaging tests by people who have had ‘abnormal’ test results from private screening. Dr Zishan Syed,
a GP in Maidstone, Kent, says the screens lead to patients ‘panicking and demanding MRI scans… often amounting to a harmless incidentaloma’, while ‘another patient who actually has a clinical indication for the scan may be delayed… The NHS can’t sustain this increasing financial pressure’.
Cholesterol levels
cholesterol blood test julian claxton jwc9767 330x330px
Screening of cholesterol levels are not recommended by the UK NSC as part of any population screening programme, although the (somewhat controversial) NHS Health Check scheme will check cholesterol in the context of a person’s overall predicted cardiovascular risk.
Yet all the health screens offered by the big private health insurers and bespoke screening companies include a cholesterol reading, again often leaving GPs to explain to anxious patients that they have nothing to worry about.
Dr David Watson, a GP in Aberdeen, says he sees ‘patients with relatively high cholesterol levels being told to see a GP but without an ASSIGN [the Scottish version of QRISK] score being calculated – which showed nothing to be done.’
Calcium testing

c0340770 blood test spl 330x330px
Many private health companies include calcium levels as part of their blood- testing packages, referring to this as a way of checking ‘bone biochemistry’ or ‘bone and muscle function’.
However, calcium testing is only ordered on the NHS for diagnostic or monitoring purposes and GPs say a finding of raised levels can be spurious out of context.
A Middlesex GP who asked not to be named tells Pulse this can result in anxiety that the patient needs to be counselled for, giving the example of ‘a marginally raised adjusted calcium in an asymptomatic young person, who Googles this and is then concerned he may have a cancer’.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.