june cover 2017
GPs may be too cynical to think that an election will focus politicians on solutions that work.
But, with patients waiting weeks for an appointment and practices closing at record levels, there was a glimmer of hope that 2017 might be different.
Because, to put it bluntly, it needs to be if general practice is to survive until the end of the next parliament in 2022.
An analysis by Pulse reveals that, if patient demand continues to grow at the present rate while GP numbers continue to stagnate, the average GP will have to work an extra clinical session a week just to keep up with demand.
In fact, even with the extra 5,000 GPs promised by the Conservatives (but strangely missing from their 2017 manifesto), GP workload would grow by two hours a week.
This is not taking into account the extra admin involved in seeing patients – which is set to increase for partners as a larger proportion of the workforce become sessional.
RCGP chair Professor Helen Stokes-tells Pulse: ‘Hard-pressed GPs around the country are already running on empty so these predictions are really concerning. As well as huge increases in the volume of patient numbers, disease management is also becoming much more complex and we simply cannot do any more without a significant injection of investment in general practice, including a significant influx of GPs.
‘We’re seeing 60 million more patients per year compared even with five years ago.’
There are solutions out there. NHS England’s GP Forward View has certainly had its critics, and rightly so. But one area it got right was that cutting unnecessary GP appointments is essential to ensure general practice can survive.
NHS England commissioned a review of 5,128 consultations across England in 2015. The report, published by NHS Alliance, estimated 27% of all appointments did not need a GP. And NHS England brought in policies to address this: changing the hospital contract to stop trusts dumping work on GPs, increasing the non-GP workforce to take on less complex appointments and reducing sick note requirements, among other things.
So far, as Pulse revealed in April, NHS England’s efforts have not yielded much: not a single hospital has been sanctioned for dumping workload on GPs, and efforts to recruit 5,000 other practice staff by 2020 have stalled, with a ‘negligible’ number of physician associates placed in practices and the number of pharmacists working in primary care slowing after a successful first year. Meanwhile, its £30m ‘Time to Care’ programme – aimed at sharing good practice in cutting workload – is unknown to many GPs.
But that is not to say this should not be a priority. Indeed, the BMA’s GP Committee chair Dr Chaand Nagpaul made this a central tenet of his keynote speech at the LMCs Conference in Edinburgh last month: ‘Liberating these one in four appointments would in effect increase GP capacity by a quarter, far greater than the political mirage of 5,000 more GPs. It’s therefore a no-brainer that the immediate priority for the NHS must be to ensure that precious GP appointments are not misused, recognising that every wasted appointment is an appointment denied to a sick patient.
‘What we need is a concerted national target to eliminate inappropriate GP workload, freeing us to care for patients who need to see us.’
Yet a Pulse analysis of the political parties’ manifestos has shown that even this ‘no brainer’ can be ignored.
Instead of a concerted effort to tackle workload – which would, after all, benefit patients who are waiting two weeks for a routine GP appointment – the parties have gone back to their favoured themes: the zombie policies that just won’t die.
Chief among the undead is seven-day routine GP access across England. The Conservatives’ manifesto not only reiterates the party’s desire for this unpopular policy, it actually brings the target forward, from 2020 to 2019.
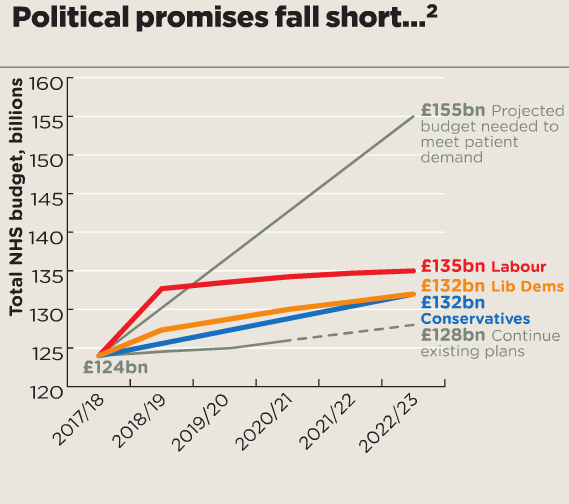
Figures box – June 2017 issue cover story
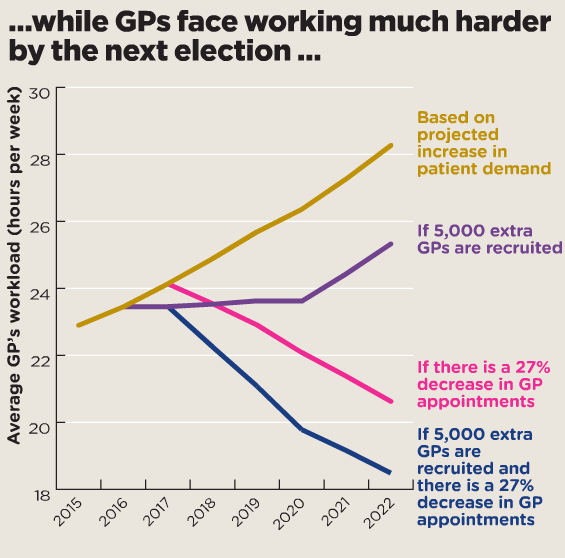
Figures box – June 2017 issue cover story
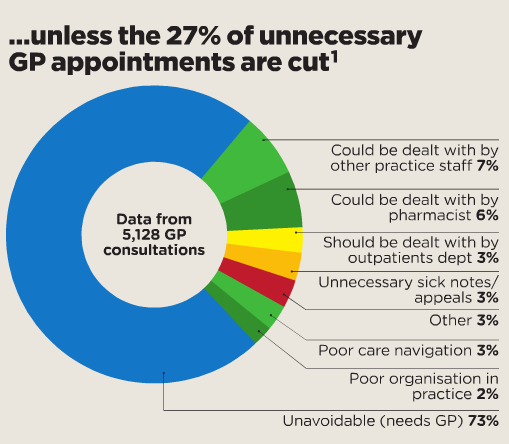
Figures box – June 2017 issue cover story
That’s not all. ‘We expect GPs to come together to provide greater access, more innovative services, share data and offer better facilities, while ensuring care remains personal… with named GPs accountable for individual patients,’ it says. ‘We will introduce a new GP contract to help develop wider public services.
Labour’s manifesto is a better read for GPs – it pledges by 2022 an additional £4bn a year for the NHS compared with the Conservatives, and says: ‘We will increase funding to GP services to ensure patients can access the care they need.’ It would also ‘scrap the NHS pay cap’ and put decisions back in the hands of the independent pay review body.
But Labour also gets bogged down in dogma, with its commitment to repeal the Health and Social Care Act, chase down privatisation and introduce a new safety regulator, ‘NHS Excellence’. The last thing GPs need in the midst of a crisis is another NHS reorganisation.
And the Lib Dems’ effort is also a curate’s egg. It emphasises the social care crisis, promises a rise in income tax to pay for health and social care, and would also end the ‘public sector pay freeze for NHS workers’ (although the ‘freeze’ was ended a few years back, replaced by a 1% cap). It promises to help vulnerable practices, offering to ‘provide national support to struggling GP practices, preventing mass practice closures’, as highlighted by Pulse’s Stop Practice Closures campaign.
Disappointingly, though – in a throwback to the Coalition days – the Lib Dems also commit to ‘expanding evening and weekend opening’.
Of course, lip service is paid in all the manifestos to ‘getting the numbers [of GPs] we need’ (Conservatives), ‘long-term workforce plans’ (Labour) and ‘ensuring we never again experience a shortage in the numbers of GPs’ (Lib Dems).
But there is no trace of the big plan to tackle this and one is desperately needed: the latest workforce figures show GP numbers fell between March 2016 and March 2017 by more than 500, despite the millions invested by the GP Forward View.
In the end, the solution will largely come down to adequate funding. And it’s true that all parties emphasise a cash injection into the NHS above current levels, with some even promising to increase spending on general practice.
But they all fall far short of what is needed. A Nuffield Trust analysis found that even Labour’s pledge – £12bn a year more by 2022/23, compared with the Conservatives’ promise of £8bn more – still falls £20bn short of the funding predicted to meet future demand.
Sadly, the cynicism of GPs is well justified. There is little in these manifestos to suggest GPs’ workload will be alleviated. And, as a result, there is every chance general practice itself could be one of the undead by 2022.
How we projected GP workload
We looked at official population projections from the Office of National Statistics up until 2022.
To assess demand, we used research by the NIHR School for Primary Care Research in The Lancet, which found that in 2013-14, the average person had 3.18 10-minute face-to-face consultations with a GP a year (increasing at a rate of 1.04% a year), 0.54 six-minute telephone consultations (12.5% a year) and 0.08 (roughly 30-minute) home visits (decreasing by 0.01 every four years).
We then split this evenly across the number of full-time-equivalent GPs, based on NHS Digital official figures and on a 44-week year, to take into account 25 days’ holiday, eight bank holidays, two days’ sick leave and five days’ study leave.
We modelled it based on two variables: whether the Government will or will not recruit 5,000 extra GPs by 2022 (starting with whether they will recruit 1,000 this year) and whether NHS England will or will not reduce appointments by 27%.
We assumed these targets would be achieved at a steady rate over the next five years.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens