Is federating putting GP practices at risk?

Federating is the panacea for general practice, or so the conventional wisdom states.
Joining together, the argument goes, is the way to protect practices from recruitment problems, enabling them to merge back-office functions and bid for contracts they would not be able to win on their own.
The BMA, Department of Health, NHS England, the devolved Governments and the RCGP are all pushing collaborative working as a way to alleviate pressure on GP practices.
There is potential for failure on a large scale
NHS England’s GP Forward View calls them ‘welcome developments we wish to see grow in coming years’, saying they provide numerous benefits, including economies of scale, sharing of best practice, opportunities to train staff, improved access and, most importantly, greater resilience. And commissioners are ploughing cash into helping practices to federate.
But federations may not be the universal cure GPs are being sold. Pulse has learned of some that are struggling or that have even gone to the wall – and some leading GPs are predicting others will follow, causing loss of money for practices and partners, and loss of services for patients.
Far from easing pressure, the federations can simply exacerbate it – leaving practices worse off than if they had stayed on their own.
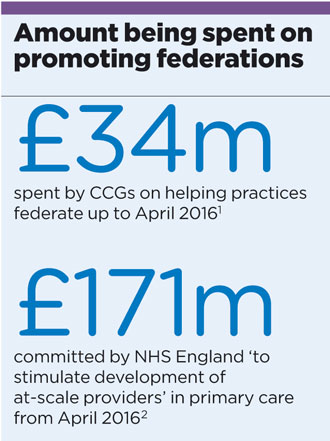
federations spend box 330x441px
For example, GPs at 54 practices have lost sums that could total hundreds of thousands of pounds through the liquidation of Bedfordshire-based Horizon Health Choices Ltd.
Member practices invested at least 65p per patient, they tell Pulse. One GP says: ‘My partners and I had invested several thousand pounds in share terms and we have lost the lot. I would never again get involved in something so large scale.’
Horizon puts the failure down to recruitment problems. It says: ‘A national shortage of GPs, particularly in Bedford, has required significant investment in locum doctors. The financial impact of this has forced the shareholders to pass a resolution to move towards liquidation.’
Elsewhere, Doncaster-based GP federation Danum Medical Services Ltd – which had held six APMS contracts – became insolvent and went into administration last March. It followed the loss of two contracts, including the region’s out-of-hours services.
A new not-for-profit community interest company called SIMUL is in the wings, ready to take Danum’s place, but Doncaster GP Dr David Coleman says doctors feel ‘burnt’ by the Danum experience and may be unwilling to get involved with federations again.
‘There’s a lot of concern because GPs have seen what can happen when it goes wrong,’ he says. ‘I imagine some practices are still uncertain as to why there is a perceived push towards working at scale, especially when we know patients value the experience at small surgeries.’
And local leaders warn more federations may be in trouble. Doncaster LMC medical secretary Dean Eggitt says: ‘I think other federations will fold as well. There is potential for failure on a large scale. The past few months have left a bitter taste here, and GPs are reluctant to get involved in federations again.’
Even those that can balance the books are facing a bumpy ride at a time of austerity. OxFed in Oxford has lost CCG funding for its team of six hybrid practice nurse/district nurse roles.
OxFed chair Dr Ben Riley stresses OxFed is a success and is breaking even, but adds: ‘You need the initial money to get going and create the structure but the more difficult bit is keeping it going. If you don’t get the commissions then it can all fall apart, which can be a disaster. People can lose their jobs.’
But that is not the story everywhere. NHS England estimates the majority of practices are now in a federation and working together can help stabilise practices. Dr Deborah Colvin, chair of the City and Hackney GP Confederation in east London, says the federation holds £11m worth of contracts, which have improved outcomes for smoking cessation, diabetes and QOF scores for long-term conditions.

dr hubertus von blumenthal 3×2
GP view: ‘In the end we were small fry in the market’
There was disappointment, anger and sadness among GPs when our federation was liquidated recently.
I was a bit sceptical when it started, and many other GPs only joined out of concern they would get left behind.
We started hearing there were problems with governance so it wasn’t that surprising when the company was liquidated. I felt there wasn’t expertise at the top or sound enough strategy. There had been some optimism but in the end the federation was small fry in the market.
Like other practices we lost money, although I don’t want to say exactly how much.
You can’t force practices to join, and the worry is that you don’t want to drag down practices that are already doing well on their own. My concern is that federations are a stepping stone towards finishing off the independent contractor status of the self-employed GP. Large healthcare companies could step in and start running them. GPs will become salaried, and terms and conditions will be dictated by private providers.
Dr Hubertus von Blumenthal is a GP in Bedfordshire and a former member of the Horizon Health Ltd GP federation
Dr Colvin says the pooling of expertise in the federation is significant: ‘We have a chief executive, finance director and other managers and so we have good governance across the practices. We also have a team containing a GP, practice manager and practice nurse who can visit and support struggling practices.’
She warns that practices that do not join partnerships, mergers or federations will not stay afloat: ‘Practices cannot survive on their own – they have to look at ways of making themselves stronger.’
The GPC certainly backs this view. Last month, it called for GP Forward View funding to be invested in collaboration between practices, as it released the results of a survey of 5,000 GPs showing 50% believe using cash to form federations or networks is a good idea.
Practices cannot survive on their own
GPC chair Dr Chaand Nagpaul says: ‘These results demonstrate a very strong desire from GPs to work collaboratively. GPs want closer ties with other practices and with multiprofessional healthcare staff. The benefits of developing these models are clear, especially as nearly four in 10 GPs believe that collaborative alliances are key to reducing bureaucracy and unnecessary workload.’
The RCGP has been promoting federations for many years, with its Roadmap for General Practice – published in 2007 – calling for ‘federated practice models’ and authored by no lesser figures than then chair-elect Professor Steve Field and 2013-16 chair Dr Maureen Baker, who was honorary secretary at the time.
Federations are also a step towards the ‘multispecialty community providers’ set out in the GP Forward View that will combine primary and secondary care.
But the income and recruitment issues that have brought down two high-profile GP federations should be food for thought: as practices in Doncaster and Bedfordshire now know, federating is not a guaranteed winner. What is presented as a panacea is not completely risk free.









