In hindsight, the 2004 GP contract was a complete financial disaster for GPs. After an initial large rise in funding, there has been a grim decade of successive cuts.
Recent figures show that last year a mere 5% of Department of Health funding went to core general practice, despite ministers’ promises of an increased allocation.
Remember the extra £5 per patient that health secretary Jeremy Hunt promised in 2014? That reached less than a quarter of practices. The £1bn infrastructure fund for primary care last year? Many bids failed, and others that were successful later had the funding withdrawn.
And while GPs wait with bated breath to see whether the latest fairytale promise will be delivered – the £2.4bn by 2020 promised in the GP Forward View – Pulse has learned CCGs have run out of patience. A Pulse investigation shows that across the country tens of millions of pounds have been ploughed into general practice, offering a rare ray of hope for a neglected profession.
Shifting the resource from secondary to community care is the way forward
Dr Graham Jackson
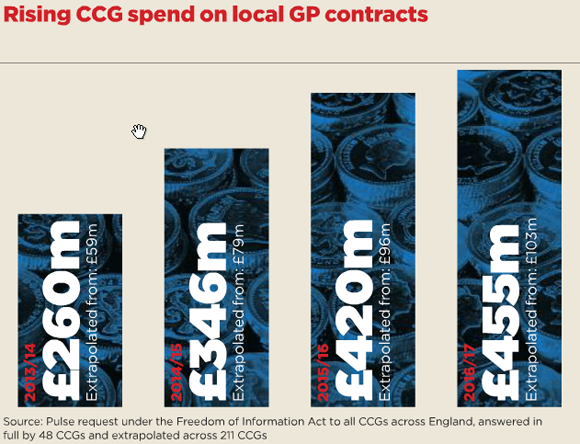
Not every area has done this – and local commissioners are expecting their pound of flesh for the investment – but among the 48 CCGs able to provide full details under the Freedom of Information Act, total spending on locally commissioned enhanced services (more commonly called direct contracts) has increased each year, from £59m in 2013/14 to £103.5m this year. Extrapolated across the country that equates to £195m of new local contracts for practices.
It appears commissioners are waking up to the idea that putting more money into general practice is cost-effective in the long term. And they are using their newly gained ‘co-commissioning’ powers to quietly shift new services – and funding – into GP practices.
Some of this funding, admittedly, has come from redirected PMS premiums and MPIG payments. But the Pulse investigation also reveals that CCGs are ploughing funding from elsewhere into general practice.
In further good news for GPs, the investigation reveals CCGs are bypassing competition for enhanced services, with only 8% of contracts being commissioned through procurement or via the ‘Any Qualified Provider’ route.

‘Good news, but we need much more’ – Read Pulse editor Nigel Praities’ latest column
Instead, CCGs are developing packages with a single pot of money for practices to provide a range of services.
NHS Bristol CCG, for example, has set up its ‘Bristol Primary Care Agreement’ – a funding pot worth £1.8m for practices. Under the wide-ranging agreement, practice clusters are tasked with providing more advanced care, such as initiating and following up dementia medication, regularly reviewing nursing home patients, diagnosing deep vein thrombosis in primary care and offering a more specialised service for patients with type 2 diabetes.
CCG spend box – August 2016 issue
Similarly, NHS Salford CCG will spend £7.6m in 2016/17 on enhanced services, up from £823,000 in 2013/14 as part of its ‘Salford Standard’ (see below). This list of 32 standards includes initiatives such as ensuring patients with severe mental illness are given annual physical health checks, assertively following up cases of non-attendance in these patients and offering longer appointments to asylum seekers.
Dr Brian Balmer, a GPC negotiator, says the shift is welcome: ‘It’s great to hear some good news for once. My experience is that most CCGs want to develop community services and GP practices – they have a real desire to develop primary care. CCGs are getting better organised, particularly when it comes to care of elderly or frail patients. They are delivering attempts to care for patients closer to home. This news is to be welcomed. It’s proof of speeches actually turning into action.’
This news should be welcomed. It is proof of speeches being actioned.
Dr Brian Balmer
CCG leaders agree. Dr Graham Jackson, co-chair of NHS Clinical Commissioners and chair of NHS Aylesbury Vale CCG, says: ‘We are seeing a shift and there is a desire for primary care investment. We know we need to invest in community care. Shifting resource from secondary care to community care is the way forward and is the best way of using that resource.’
NHS Dorset CCG tells Pulse it was able to increase funding to £9.1m this year – up from £5.12m in 2013/14. It was one of the only areas to continue the £5 per patient scheme, and has also invested £3.9m in ‘over 75s locality development schemes’, requiring practices to submit plans detailing how they intend to keep older vulnerable patients out of hospital.
Dr Nigel Watson, chief executive of Wessex LMCs and former chair of the GPC’s commissioning subcommittee, says: ‘We negotiated with NHS Dorset CCG. Not only did they reinvest the PMS premium, they matched that funding.’
He adds that the GPC is pushing for CCGs to pool enhanced service funding and offer practices a block contract. Dr Watson says: ‘We need to identify what is outside GMS, but make that simpler to deliver, rather than have 15 different contracts that are all small pots of funding. We would like to see it packaged up as one pot, such as is happening in Bristol, Salford and Dudley.’
Dr Jackson says his CCG is looking to package up the funding in the same way to avoid the old-fashioned concept of ‘bean counting individual items of service’. He says: ‘By bundling contracts together, you audit against that and get the product without the administration.’
But, before we crack open the champagne, there may be trouble ahead.
As Dr Watson puts it: ‘Some CCGs are more able to invest than others.’ And 39 CCGs finished the last financial year in deficit.
Ominous developments
Pulse has reported on a number of CCGs that, instead of extending care, are rationing front-line services such as treatment for smokers and obese patients, hearing aids, IVF treatment and vasectomies. Others are even encouraging GPs to stop prescribing over-the-counter medicines in a bid to cut costs.
And there is another danger looming. In recent months there have been several influential voices calling for mergers – or even the complete abolition – of CCGs to save money. If yet another round of NHS reorganisation comes – a mere three years after the last one – then all this progress could be squandered.
Secret ‘sustainability and transformation plans’ (STPs) have been drawn up across England under NHS ‘shared planning guidance’. They are currently being scrutinised by NHS bosses. These plans involve health and care services being planned by geographical area, rather than around individual organisations, and are likely to contain some radical cost-saving measures to ensure the health service comes back to financial balance.
If the STPs result in cuts to general practice budgets then the all the ‘good news’ initiatives above could be in vain.
Salford: Longer appointments for asylum seekers
GPs in Salford will be incentivised to offer longer appointments to asylum seekers as part of a contract being offered by NHS Salford CCG.
The indicator relating to asylum seekers requires practices to record patients’ asylum status, accommodate cultural requirements, for example by offering a choice of a male or female GP, use translation services and refer those with mental illness to a specialist service.
This is one of 32 elements of the ‘Salford Standard’ – a set of indicators worth £7.6m that replaces a host of enhanced services with GP practices this year. CCG chair
Dr Hamish Stedman says: ‘A key aim is to level the playing field for primary care in terms of investment and improve quality of care.’

asylum seekers in waiting area SUO 580x200px
Blackburn and Darwen: GPs consulted on how to spend £6m
NHS Blackburn and Darwen CCG has launched a five-year scheme to support primary care. It has asked its GPs to work together to devise a plan for a proposed £6m investment in primary care services, pooling all the money spent on current enhanced services, such as those for prescribing in the elderly and boosting uptake of bowel cancer testing.
CCG chief clinical officer Dr Chris Clayton says: ‘There was a recognition… that spending was not as balanced as it should be between primary care and secondary care. We are now bringing all the enhanced service schemes together in one place.’

money SUO 580x200px
Rotherham: GPs to staff new ‘emergency centre’
NHS Rotherham CCG has been able to shut three wards in its local hospital because of additional services provided in general practice.
Practices have been incentivised to set up multidisciplinary teams, put admission-prevention plans in place and discuss all care home admissions. The CCG will also open an ‘emergency centre’ in 2017, which will be partly staffed by GPs with senior triage staff, to address acute care needs in the community.
The CCG’s total investment in enhanced services has risen from £2.3m in 2013/14 to £3.6m this year. Chair Dr Julie Kitlowski says: ‘Patients want care closer to home. We would aspire to put even more money into primary care but there are issues around recruitment and retention.’

empty hospital ward SUO 580x200px
Hertfordshire: GP ‘ward rounds’ in care homes
GPs are expected to offer the ‘equivalent of ward rounds’ in care homes as part of a revamped enhanced service in Hertfordshire.
The care home enhanced service offered by NHS East and North East Hertfordshire CCG has more than trebled in value since 2013/14, from £220,000 to £774,000.
The CCG’s overall spend on enhanced services has also more than trebled since 2013/14.
CCG chief executive Beverley Flowers says: ‘Care of the elderly and the frail has been our real drive. We are offering an enhanced GP service in care homes, and have encouraged GP practices to build relationships with care homes and offer the equivalent of ward rounds. It is a more structured approach.’

care home SUO 580x200px
What are local authorities doing?
Sadly, local authorities do not appear to have got the memo on prioritising general practice. A request under the Freedom of Information Act, answered in full by 59 of 150 councils, revealed a slight fall in public health contracts with GP practices in 2016/17 to £102.1m across England, compared with £104.3m last year and £112.5m in 2014/15. This is not a complete surprise as austerity bites. Pulse has revealed funding cuts for GP-based smoking cessation and sexual health services.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












