Terrible toll: How GP closures have worsened in the past year


cover story April 2017 3×2
A year ago, with general practice on its knees, NHS England came through with a five-year programme intended to pull it out of the crisis.
‘This will turn general practice around,’ proclaimed NHS England chief executive Simon Stevens on the front page of Pulse.
There were to be year-on-year increases in core practice funding, alongside a £500m ‘turnaround package’ of measures to shore up practices.
The GP Forward View package was clear: this money would ‘help further support struggling practices in the interim, develop the workforce, stimulate care redesign and tackle workload’.
But one year on and familiar problems persist: GPs’ workload is still too high, the recruitment crisis hasn’t gone away and demand continues to increase.
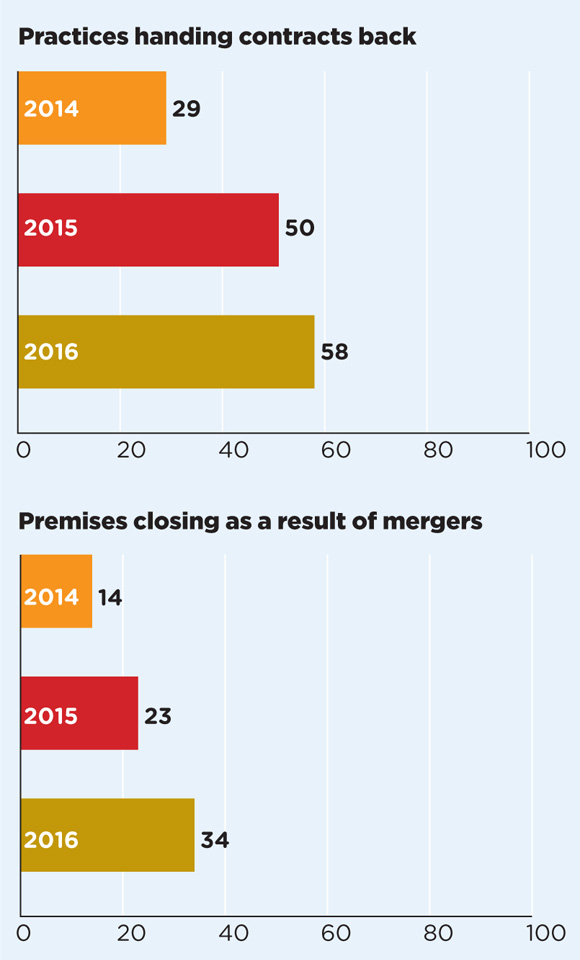
Perhaps most damningly, the number of practices closing – with devastating effects on GPs, staff, patients and neighbouring practices– has actually gone up.
Shockingly, a Pulse investigation shows last year almost a quarter of a million patients had to move practice due to practice closures or mergers in England.
This is up on 2015 and dwarfs the number of patients affected by closures in 2014 – an increase of 150% in two years – and the total number of GP premises closed is up a quarter in the past year.
CCGs have not delivered the resources available
Dr Chaand Nagpaul
Some areas have been particularly badly hit. Brighton, for example, has seen seven practices close in the past two years – including four closures that have displaced a total of almost 9,000 patients since the GP Forward View was announced last April. Other areas are teetering on the brink. Pulse has reported that practices across the whole Yorkshire town of Bridlington have closed their lists to new patients due to fears of the domino effect a potential practice closure would cause.
It wasn’t meant to be this way. The pots of funding were significant: a £40m ‘practice resilience fund’; £206m to grow the medical and non-medical workforce; £171m to be spent by CCGs on ‘practice transformational support’; and £30m to spread innovation to release GPs’ time.
Admittedly, this funding is spread over five years, but since the package was announced 12 months ago the money has been very slow to come on stream.
The ‘transformation fund’ has not yet started, workshops designed to reduce GP workload conversely had the effect of taking up more time for GPs, and – despite considerable focus and investment this year – the GP workforce actually contracted last year.
NHS bosses have recently started to rush through £16m of resilience support for practices on the brink, but the evidence so far is that general practice has some way to go before it is stabilised. Quite the opposite – things are getting worse.
In 2015, 73 GP premises had to close as a result of partners handing contracts back or merging. This rose to 92 in 2016. The number of patients having to change practices as a result went up by 17%, from 221,000 to 259,000.
Despite this, a BMA survey of LMCs found that, as of February 2017, 38% of regions reported their practices had not received any funding or support through the practice resilience scheme.
Even the RCGP – a key cheerleader for the GP Forward View – has been unimpressed. In January, it ‘red rated’ NHS England’s progress on aiding vulnerable practices, having found that less than a fifth of the fund had been spent by NHS regions in the eight months after it was announced.
NHS England says the full amount has now been ‘committed’, but GPC chair Dr Chaand Nagpaul is indignant: ‘We know the money, targeted in the right way, for the most severely affected practices, can make a difference.
‘The tragedy is CCGs have not delivered their part in making the resource available. Many practices that should have received support have had none to date. That’s been a failing of local delivery.’
Practice closures continue
april 2017 practices closures 1 revised

april 2017 practices closures 2 revised
NHS bosses were slow to learn the lessons of a similar £10m scheme launched before the GP Forward View to help vulnerable practices. This funding has only just been spent – two years after it was first announced – despite Pulse having, under its Stop Practice Closures campaign, continually highlighted that the cash was not getting to the front line.
Speaking at the Pulse Live conference in London last month, NHS England’s head of general practice development Dr Robert Varnam admitted that the 2015 fund had been an ‘excruciating disappointment’, with money taking too long to reach practices.
However, he added that the systems for getting money to vulnerable practices are totally different now from when it was launched, ‘learning from those appalling lessons which were genuinely desperate’.
Dr Nagpaul says: ‘There are some parts of the country where the money had been made available last year and been put to good effect. But there are other areas – including some parts of London – where practices have not even been notified of payment, and others where it has been paid at the last minute.
‘We’ve had meetings with NHS England central, and it is not to do with them – they are very clear that they want this money spent. The problems are local.’
It seems as though the money is finally starting to filter through. As of 29 March, £9.2m of the £10m 2015 fund has been spent, and £11.9m of last year’s £16m fund. In total, 1,100 practices have benefitted, NHS England claims.
But it has been done in a rush. For example, in Stoke, the 14 practices that asked for funding were each given £10,000-plus lump sums in late February.
Other LMCs – such as Doncaster and Bedfordshire and Hertfordshire – were only informed this year how much funding practices will receive, leaving them with little time to work up plans that will benefit vulnerable practices.
Meanwhile, practices in Walsall were given just two days to submit bids after the regional team sat on the funding. Walsall LMC medical secretary Dr Uzma Ahmad tells Pulse: ‘We didn’t hear anything from them for five months. Then practices were given a couple of days to decide whether or not to accept the offer, which would also involve stumping up some money themselves.
‘We had six practices that were given approval for funding. Three have not accepted the offer as it was such a rush.’
Dr Dean Eggitt, medical secretary of Doncaster LMC, says GPs in the region have now been given funding ‘in a rush’, which is being used to set up a federation.
He adds: ‘There is some “slippage money” – they haven’t been able to spend it in-year, so there is a rush to get rid of it now.
‘Either local areas need to think ahead of time what plans they have in the drawer, or we need to get rid of this preposterous idea of raking back cash at the end of the year.’
For its part, NHS England says it is ‘perverse’ that it has been ‘accused of allocating this money both too slowly and too quickly’. A spokesperson added: ‘Instead we’re focusing on ensuring the funding achieves the maximum benefit for both GPs and patients.’
But surely a fundamental barometer of the success of the rescue package is stabilising practices and reducing the rate of closures? By this measure alone, the GP Forward View has made scant progress in its first year.
It’s not all doom and gloom
The GP Forward View may have been a bit slow off the mark, but around the country LMCs are also stepping in to help.
Efforts by Londonwide LMCs – with no help from the resilience fund – have saved dozens of practices. Chief executive Dr Michelle Drage tells Pulse: ‘We can confidently say that last year our assistance helped the equivalent of around one practice a week through significant, serious risks to their contracts.
And, to be fair to NHS England, there is still the bulk of a £500m package of support to come over the next four years including £24m of practice resilience funding.
Pulse has received reports that practices receiving resilience funding – albeit late – have said it has saved them from potential closure, for example by allowing them to plug staffing gaps.
If managers can ensure all this money quickly gets to the practices that need it, then the profession might finally see the steady stream of practice closures start to slow.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens











