A moral dilemma: GP practices offered incentives to cut urgent referrals


Practices are being given money to cut the number of referrals they make.
An FOI investigation by Pulse has learnt that in at least nine CCGs, practices are being offered large payments for keeping within targets for outpatient referrals and follow-ups.
And some of these schemes even count emergency admissions and two-week cancer wait referrals towards their target.
Such schemes are not new – in 2012 former GPC chair Dr Laurence Buckman reported PCTs’ schemes to the GMC, declaring: ‘Taking money from patient care and pocketing it for reducing something you do is wrong.’
But CCGs are now also increasingly using them to cut costs, in the shadow of a £22bn black hole in NHS finances.
The GPC says many of these schemes are ‘ethically questionable’ and Pulse has learned that the GMC looked into at least one of them to see if it is contrary to the guidance set out in Good Medical Practice.
However, it is the inclusion of urgent cancer referrals that has caused most controversy. NHS Lambeth CCG is offering payments for practices moving towards the average 2014/15 CCG referral rate per 1,000 patients.
The CCG claims that urgent care and two-week cancer referrals ‘cannot be separated’ from the overall numbers.
The same is true in NHS North-East Lincolnshire CCG, where the average practice is being offered the equivalent of more than £6,000 to reduce outpatient referrals to the same level as the 25% of practices with the lowest referral rates – including two-week urgent cancer referrals – in 2014/15.
Dr Emma Rowley-Conwy, a GP in Lambeth, south London, says that such targets are ‘counter to other initiatives that encourage GPs to refer earlier for suspected cancers’.
Former RCGP chair and Lambeth GP Professor Clare Gerada tells Pulse she believes such schemes risk ‘interfering with the doctor-patient relationship.’ She says: ‘Once we start incentivising to reduce activity, then it puts a conflict within the consulting room.’
And the GPC goes even further. Dr Robert Morley, chair of the GPC’s contracts and regulations subcommittee, tells Pulse these two schemes are ‘extremely concerning’, adding ‘I wonder what the GMC would think’.
Dr Morley says that all the schemes identified by Pulse have question-marks hanging over them.
He says: ‘These may, at face value, potentially be ethically questionable and conflict with GMC guidance, on the basis that they might conceivably influence individual management decisions.’
The GMC said this could be regarded as an inducement if it changed GP behaviour
Dr George Ogden
Indeed, one LMC has alerted the GMC about its local scheme. Dr George Ogden, chair of Bolton LMC, tells Pulse that the LMC fears that NHS Bolton CCG’s ‘quality contract’, which replaced all local enhanced services, could fall foul of the GMC’s guidance.
Under the NHS Bolton CCG ‘quality contract’, practices will receive payment for reducing referrals for procedures of limited clinical value by 20% – such as vasectomies – and for reducing first outpatient appointments and follow-ups by 1%. It has identified more than £150,000 in savings to be made on tonsillectomy, hysterectomy and myringotomy procedures and says it ‘sought GMC guidance’ before implementing the scheme.
Dr Ogden says: ‘The GMC said it would potentially be regarded as an inducement if there was a challenge that GP behaviour changed as a result of the payment. So they were concerned, but didn’t say it was entirely against the guidance.’
Good Medical Practice states that GPs must not accept ‘any inducement, gift or hospitality’ that may affect the way patients are referred (see box).
NHS Birmingham South Central CCG is offering the average practice a equivalent payment in excess of £11,000 to reduce new outpatient attendances, follow-ups, A&E attendances and emergency admissions by 1%, compared with 2014/15. The CCG says it has considered the ‘full impact’ of the incentive scheme and is ‘confident that there is no conflict of interest’.
But it is the public perception of these payments to reduce referrals that is of particular concern, in the wake of the furore over NHS England’s ‘cash for diagnoses’ drive last year, whereby practices were paid £55 for each newly diagnosed case of dementia.
Reputational risk
Dr Tony Grewal, medical secretary at Londonwide LMCs, says that although he does not think GPs will change their behaviour, he is worried about the ‘reputational risk’ if patients think GPs are making decisions based on their own self-interest.
Dr Grewal says: ‘I’ve got no concerns in terms of what GPs are actually doing or for patient safety. My only concern is the perception that this could be interpreted as GPs being paid not to refer.’
In the capital, at least six CCGs – including NHS Lambeth CCG – are offering incentives for practices to reduce referrals. In NHS Hammersmith and Fulham CCG, a total of £107,600 is available across all practices for ‘referral variation reduction’, with more than a third of the funding linked to hitting practice referral targets in 10 ‘high-activity areas’ – although they declined to say what these are.
Neighbouring NHS West London CCG has set practices a target of no more than 272 outpatient appointments (including follow-ups) to all secondary care specialties per 1,000 registered patients.
NHS Sutton CCG says practices receive 22p per patient for reducing referrals, which can be spent as they wish. Commissioners say the schemes are not creating a conflict of interest, with NHS North West London Collaborative CCGs – which includes NHS Hammersmith and Fulham CCG and NHS West London CCG – saying they are only targeting ‘inappropriate referrals’.
CCGs also point out targets are part of wider schemes to reduce referral rates, which focus on practices’ processes.
Dr Michael Dixon, chair of the NHS Alliance, says the incentives may be one of the only mechanisms CCGs have to meet budget constraints.
He says: ‘CCGs are having to keep within budget in a terribly unfair system, which has seen all the money going into secondary care, with hospitals incentivised to boost activity, because they’re paid by activity. So the only counter for CCG would be with GPs conscientiously trying to avoid referral and the use of hospitals unnecessarily.’
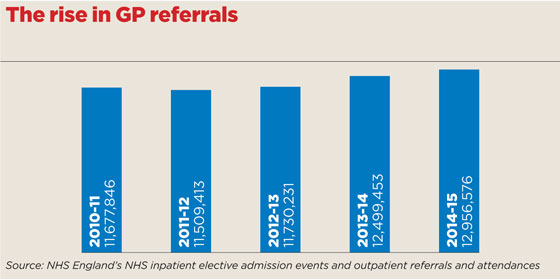
To back this up, in common with all areas of NHS activity, GP referrals are increasing – by 11% since 2010/11.
But regardless, it was never meant to be this way. At their inception, CCGs were championed as clinically led organisations that would avoid the potentially inappropriate methods used by their forebears at PCTs. However, circumstances seem to be exposing them as mere chips off the old block.
What does the GMC say?
Good Medical Practice says: ‘You must not ask for or accept – from patients, colleagues or others – any inducement, gift or hospitality that may affect or be seen to affect the way you prescribe for, treat or refer patients or commission services for patients. You must not offer these inducements.’
When approached by Pulse about our investigation, GMC chief executive Niall Dickson said that although financial and other incentives ‘can be an effective way of driving improvements’, GPs needed to avoid falling foul of regulations. He added: ‘[GPs] need to satisfy themselves that the scheme will benefit their patients and that there is flexibility to meet the needs of individuals. If a doctor does have concerns about a scheme, they should raise their concerns.’
What are GP practices being paid to do?
NHS Bolton CCG
A ‘quality contract’, which includes rewards to practices for reducing by 20% procedures of low clinical value, such as vasectomies, hysterectomies and myringotomies, and for reducing first outpatient appointments and follow-ups by 1% each. The CCG states: ‘This is a quality standard which aims to ensure that patients receive the right treatment at the right time. What can be managed in primary care, will be.’ It added that it had ‘sought guidance from the GMC before implementing the contract’.
NHS Birmingham South Central CCG
The CCG’s incentive scheme offers practices a maximum payment of £1.60 per patient for staying within 1% of their 2014/15 activity in four areas: new outpatient attendances; follow-up outpatient attendances; A&E attendances; and emergency admissions. A CCG spokesperson told Pulse it had considered the ‘full impact’ of the scheme and was ‘confident that there is no conflict of interest’.
NHS Sutton CCG
The GP engagement scheme includes incentives for keeping within a target (245) per weighted 1,000 population for all first outpatient referrals in 2015/16. Funding amounts to 22p per head of capitation for achievement of the target.
NHS North East Lincolnshire CCG
Practices can earn a maximum payment of 90p per patient for improving or maintaining all outpatient referral activity levels against their performance in 2014/15. The scheme encourages practices to reduce or maintain referrals in line with the top 25% with the lowest referrals in 2014/15. This includes referrals under the two-week cancer pathway.
NHS West London CCG
The CCG has set a ‘target rate’ for practices of a maximum of 272 hospital appointments per 1,000 practice population, including all follow-up attendances. It also has a target of 60 per 1,000 non-elective admissions. The appointments target excludes specialties covered by QIPP targets: diabetes, cardiology, rheumatology, respiratory, ophthalmology. The CCG said: ‘Practices whose rate per 1,000 is above the target line will be required to reduce to the target line to achieve full outcome payment.’
NHS Hammersmith and Fulham CCG
The CCG has made £107,600 available to all practices for ‘referral/variation reduction’, with a quarter of the funds paid for hitting targets for referrals to four high-activity specialties, which it declined to specify. A further third is available for bringing referrals in line with CCG-level targets per 1,000 patients.
NHS Bexley CCG
It floated the idea of a referral management scheme at the start of the year, considering the ‘introduction of locality budgets for elective activity, which will reward more effective management by practices’. It has since launched a review of key areas of demand for referral and activity levels.
NHS Lambeth CCG
The CCG has agreed a contract with GP federations to review variation and last year targeted GP-initiated first outpatient referrals to individual specialties. Under the contract, 35% of the overall payment is linked to practices moving towards the average CCG referral rate per 1,000 patients in 2014/15.
NHS Enfield CCG
The CCG hasn’t set practice level targets, but there is a financial incentive payment to practices if their locality – of which Enfield has four – comes in under target for first outpatient referrals, A&E attendances and over-65s’ emergency admissions.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












