Case 1
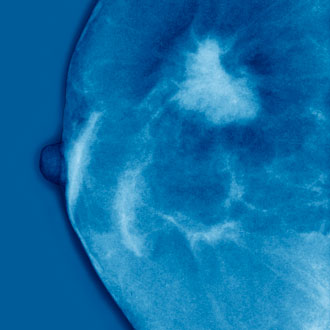
Ms S, a 39-year-old teacher, consulted the practice nurse with discomfort in the left breast and stickiness on the nipple. She was seen by one of the GPs the same day, who recorded that there was a slight white discharge from the left nipple but no lumps. Three months later she returned to the group practice, saying that the left nipple retracted intermittently and there was some eczematous change but no lumps. She was again reassured and given topical steroid cream. One year after first presentation she saw a new GP, who referred her urgently to the breast clinic.
After triple assessment she was diagnosed with invasive carcinoma, treated by modified radical mastectomy. Histology confirmed Paget’s disease of the nipple with an underlying grade III, HER2 positive cancer and heavy axillary nodal involvement.
GP diagnosis
Non-specific dermatitis
Actual diagnosis
Paget’s disease of the nipple
Clues
Any eczematous change restricted to the nipple/areola may be a sign of Paget’s disease, which is almost invariably associated with an underlying cancer, either invasive or non-invasive (DCIS).
Take home message
Refer every patient with nipple eczema who has no other evidence of eczema for assessment. Topical steroids can produce temporary improvement in Paget’s disease.
Case 2
Mrs C, a 67-year-old retired shop assistant, consulted her GP with a tender right breast lump. She was known to have breast cysts and had been taking HRT for 22 years. After finding cystic changes in the left upper outer quadrant and a painful lump on the right side, the GP made a diagnosis of a cyst because of the prior history, and tried to persuade her to stop HRT. The patient wanted to continue HRT, but agreed to try evening primrose oil. Six months later, she consulted another GP with the same right breast lump. There was a 1.5cm lump lateral to the right areola, with another lump medial to this, and she was referred urgently to the breast clinic. After triple assessment, she was diagnosed with a right breast cancer with axillary nodal involvement.
GP diagnosis
Breast cyst in postmenopausal woman taking HRT.
Actual diagnosis
Breast cancer, amid breast cysts.
Clues
Women who develop multiple breast cysts are at increased risk of breast cancer, as are women taking prolonged HRT.
Take home message
Do not assume that a new lump in a woman with a history of breast cysts is another cyst.
Case 3
Ms T, a 42-year-old hairdresser, consulted her GP with a tender area below the left nipple which had been troubling her for a week. There was slightly tender nodularity deep to the left nipple. She was given erythromycin and asked to return in two weeks if it had not settled. When seen at that time she was pain-free, but was not re-examined by the GP. She moved to a new house and consulted her new GP six months later, complaining of a lump behind the left nipple. She was referred urgently to the breast clinic and a left central breast lump was found. After triple assessment, she was diagnosed with invasive breast cancer. She underwent left mastectomy and axillary clearance for a grade III carcinoma with nodal involvement.
GP diagnosis
Mastitis
Actual diagnosis
Breast cancer
Clues
An asymmetric abnormality was present. Clinical examination would have revealed that this was the case.
Take home message
If a patient has been asked to return for evaluation of an asymmetrical breast abnormality, clinical examination is mandatory. Either persistent nodularity or a lump requires assessment in a breast clinic.
Case 4
Mr P was diagnosed with large cell anaplastic non-Hodgkin’s lymphoma in 1998, aged 49. He received chemotherapy, vincristine, adriamycin, prednisone, etoposide, cyclophosphamide and bleomycin (VAPEC-B), followed by radiotherapy to the para-aortic region and left pelvis. After this, he developed loss of libido.
In January 1999, a 3cm tender lump in the left breast was diagnosed as gynaecomastia. He remained under follow up until 2003, with no evidence of recurrence.
In June 2009, aged 61, he injured his left nipple and consulted his GP, who noted that the nipple was indurated, but thought it had always looked like that since he received chemotherapy. He was reviewed in July and August, when he was reassured about the left nipple inversion.
Approximately 18 months later, he noticed a lump in his left armpit, and a new GP noted a left breast lump and two enlarged lymph nodes in the left axilla. Two weeks later, he was seen in the breast clinic, where it was found that there was an ulcerated carcinoma of the left breast with skin nodes extending to the left axilla. There were metastatic feeling nodes in the left axilla, right-sided gynaecomastia, and hepatomegaly with the liver edge five finger breadths below the costal margin. Ultrasound of the breast confirmed multiple malignant-looking lymph nodes, and liver ultrasound showed diffuse infiltration with metastatic disease. Cytology from the axilla confirmed the presence of malignant cells (C5). A punch biopsy from the left breast showed invasive lobular carcinoma (ER/PR/HER2+ve). A CT scan revealed extensive sclerotic bony metastases and diffuse liver infiltration. He was started on palliative letrozole.
GP diagnosis
Gynaecomastia
Actual diagnosis
Advanced male breast cancer
Clues
- Longstanding testicular failure
- Increase in size of breast mass
- Skin ulceration
Take home message
In a male with long-standing gynaecomastia an increase in size or skin ulceration is sinister and warrants urgent referral
Professor Ian S Fentiman is emeritus professor of surgical oncology at Guy’s Hospital, London
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens