GP Dr Louise Tulloh and cardiologist Professor Robert Tulloh discuss this case of palpitations in a 13-year-old girl
Case
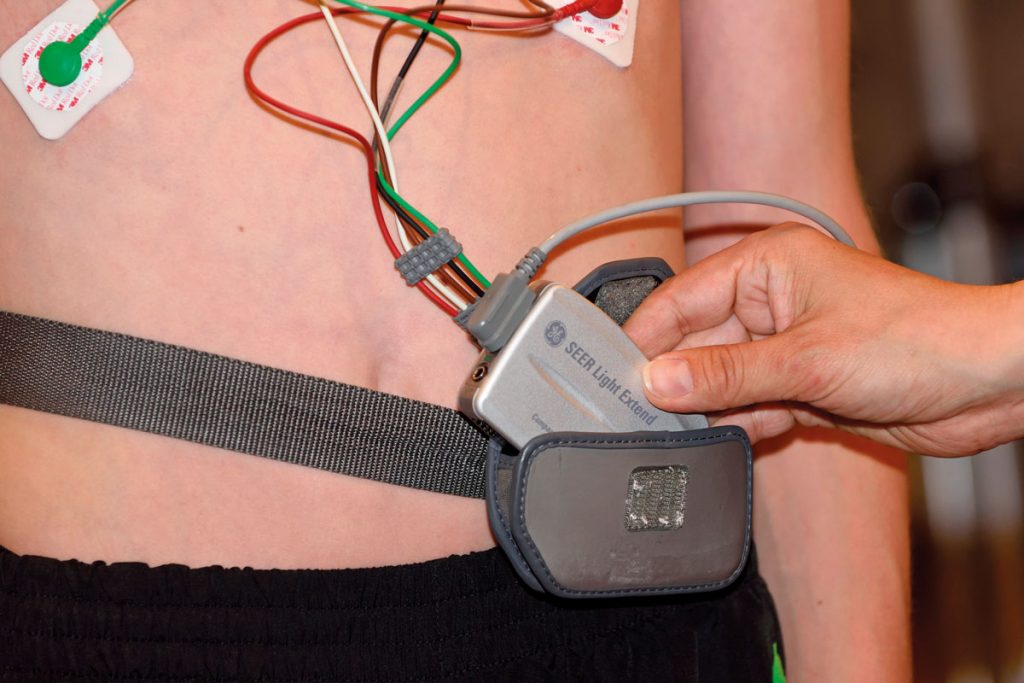
A 13-year-old girl presents to her GP with episodes of fast palpitations. Her ECG looks abnormal. Her GP suspects an underlying arrhythmia and refers her to cardiology.
The problem
Wolff-Parkinson-White (WPW) syndrome is a type of supraventricular tachycardia and affects up to three in 1,000 people worldwide. Patients with WPW are born with an additional electrical conduction pathway between the atria and the ventricles.1 This allows the atrioventricular node and the bundle of His to be bypassed and conducts atrial depolarisations directly and quickly to the ventricles. There are some forms that are close to or even within the atria-ventricular node. It is a type of pre-excitation syndrome.3
Generally, the underlying cause of WPW remains unknown.2 Some cases are genetic, inherited in an autosomal dominant fashion and attributed to a mutation of the PRKAG2 gene.2 It is also rarely associated with a congenital heart condition called Ebstein anomaly,1 where babies are born with the tricuspid valve leaflets displaced apically onto the walls and septum of the right ventricle. This results in a large right atrium and a small right ventricle along with a very leaky tricuspid valve. Most cases of WPW, however, occur sporadically, in people with no known family history.2
Features
Paroxysmal supraventricular tachycardia is the most common arrhythmia associated with WPW.1 WPW is characterised by episodes of tachycardia and ECG evidence of ventricular pre-excitation in between episodes.
People with WPW may be asymptomatic. If symptoms do occur, they can include palpitations, syncope, dizziness, breathlessness, sweating and chest pain. Rarely, cardiac arrest and sudden death may occur.1
Symptoms can be brought on by exercise, caffeine or alcohol, but usually occur at rest and can last from a number of seconds to several days. Some patients may experience frequent symptoms (several times a day) whereas others suffer infrequently (every few months).
Diagnosis
Diagnosis is made on the symptoms and family history. Typical presentations include sudden onset and offset of palpitation, often lasting a few minutes or longer. The patient is typically at rest, episodes almost never occurring on exercise. The heart rate is very fast (‘too fast to count’) and the patient may feel light headed and look pale during an episode. This is very different from an extra beat – or ‘bump’ in the chest. The 12-lead ECG will reveal a delta wave, which is a slurred upstroke of the QRS complex, associated with a short PR interval.3
The short PR interval (less than 120ms in duration in adults, less than 80ms in children), widened QRS complex (greater than 120ms in duration) and slurred upstroke of the QRS complex are the classic features of WPW.
Routine investigations
ECG abnormalities in WPW include:
• A wide and initially slurred QRS complex (delta wave).
• A short PR interval.
• During episodes of supraventricular tachycardia, P-waves and delta waves are lost and the QRS is normal.
• Often there is a dominant R-wave in lead V1 and an inverted T-wave in the anterior chest leads.
Management
In some cases, formal treatment is not required. Vagal manoeuvres (techniques that stimulate the vagal nerve and slow the heart rate), such as the Valsalva manoeuvre, where the patient pinches their nose, shuts their mouth and exhales hard while straining, can be helpful to terminate episodes of tachycardia.
Chemical cardioversion can be obtained using adenosine. This is given via a fast intravenous injection at increasing doses while monitoring the ECG. Electrical cardioversion can also be required. It delivers a dose of synchronised electric current to the heart, aiming to restore normal electrical activity.
Management of recurrent SVT due to WPW can be achieved by using antiarrhythmic medication like β-blockers or calcium channel blockers.
Other options include ablation procedures – where a cardiac catheter is used to direct radio-frequency energy (heat) or cryoablation (cold) to the accessory electrical pathway, thereby destroying the aberrant tissue. This can help restore sinus rhythm and is highly successful.2
Atrial fibrillation associated with WPW can be dangerous, sometimes leading to ventricular fibrillation. Some people with WPW may be predisposed to cardiac arrest or sudden cardiac death, due to a number of influences including highly complex aberrant intracardiac conduction pathways.2 It can be treated with cardioversion or medication.
To prevention future episodes of AF, drugs such as oral sotalol and amiodarone are known to be effective or else ablation as above. The long-term prognosis for individuals with WPW is excellent due to the treatment options.
Dr Louise Tulloh is a GP in Bristol. Professor Robert Tulloh is a professor of congenital cardiology and pulmonary hypertension at the Bristol Heart Institute
References
1
US National Library of Medicine Genetics Home Reference. Wolff-Parkinson-White syndrome. 2017 ghr.nlm.nih.gov/condition/wolff-parkinson-white-syndrome
2
National Center for Advancing Translational Sciences, Genetic and Rare Diseases Information Center. Wolff-Parkinson-White syndrome. 2012. rarediseases.info.nih.gov/diseases/7897/wolff-parkinson-white-syndrome
3
Bhatia A, Sra J, Akhtar M. Preexcitation Syndromes. Current Problems in Cardiology. 2016;41: 99-137. doi:10.1016/j.cpcardiol.2015.11.002. PMID 26897561.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













