GP Dr Marion Sloan considers this rarely seen presentation
What is it?
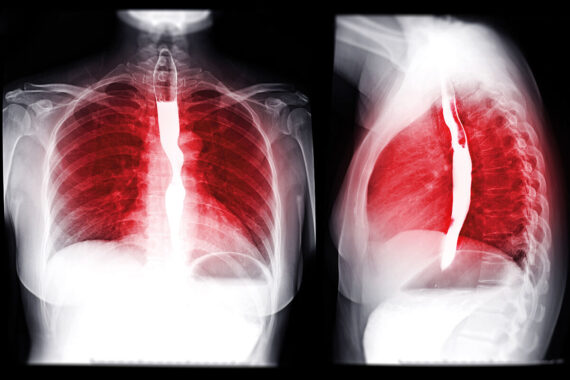
Achalasia is a rare swallowing disorder. The cause is unknown but it can be inherited, autoimmune or postviral. It is the result of dysfunction of the nerves in the oesophagus. Peristaltic activity is lost and the lower oesophageal sphincter cannot relax and allow the passage of food into the stomach. The oesophagus becomes dilated as it overfills. The stagnant column of food and fluid causes acute inflammation of the oesophageal epithelium.
Achalasia usually presents in adults, but some cases are genetic and can present in childhood. Sometimes the condition is asymptomatic, but diagnostic features develop as the disease progresses. These can be chest pain, reflux, heartburn, nausea, vomiting, dysphagia and weight loss. Undigested food may be regurgitated. Patients may aspirate food, causing recurrent chest infections. The patient becomes debilitated, loses weight and feels tired all the time. Rarely, achalasia presents as an emergency where the overstretched oesophagus bursts and its contents flow into the thoracic cavity.
How rare is it?
Incidence is one case every 100,000 patient years.
May be confused with…
The diagnosis can be confused with angina, reflux, a pharyngeal web, oesophageal spasm, heartburn, non ulcer dyspepsia, hiatus hernia and cancer of the oesophagus. Furthermore, conditions can co-exist.
Red flags
Dysphagia and weight loss are red flags, and warrant a two-week-wait referral.
Clues for early detection
Other diagnostic features of achalasia overlap with innocent conditions, so achalasia can go undetected for long periods.
A strong clue is dysphagia for liquids. Another is when the patient’s family complains about how slowly they eat and maybe laughs at the contortions and position changes the patient uses to achieve a swallow.
If a patient has debility, weight loss, general deterioration or general loss of wellbeing, combined with swallowing issues of any sort, it’s time for further investigation. Tests may include endoscopy, a barium swallow to illustrate the distended oesophagus, or high-resolution manometry, which will confirm the abnormal peristaltic activity.
Treatment and prognosis
Primary care treatment could include muscle relaxants such as long-acting nitrates and calcium channel blockers to lower pressure in the distal oesophageal sphincter.
Secondary care treatment incudes balloon dilatation, under sedation or a general anaesthetic, where a small balloon is passed through the endoscope and inflated at the lower oesophageal sphincter to stretch and split some of the muscle fibres. Botox can be injected endoscopically. An alternative is a peroral endoscopic myomectomy (POEM) procedure. Endoscopic management has largely superseded the laparoscopic Heller’s myotomy operation.
There is currently no cure for achalasia.
The patient needs ongoing secondary care review as cancer of the oesophagus is a rare but late complication. Dietitians can optimise nutrition. Tips to remain well-nourished include chewing well, eating slowly, washing each mouthful down with a fizzy drink, sitting upright to eat and not eating late at night. Sleeping upright on several pillows may help. With these measures the prognosis is good.
Researchers at University College London Great Ormond Street Institute of Child Health are looking at injection of stem cells into the oesophagus in the hope of generating new nerve cells to restore normal peristaltic function.
Dr Marion Sloan is a senior GP partner at Sloan Medical Centre, Sheffield, chair of the Primary Care Society of Gastroenterology and a GP hospital practitioner at Sheffield Teaching Hospitals performing endoscopy
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens