Ten top tips – Inflammatory bowel disease
Have a low index of suspicion for IBD in patients with a family history or extraluminal symptoms
1. IBD runs in families and is not just a luminal disease
There is a 10-fold increased risk of IBD if there is any family history and a 30-fold increased risk if a sibling has IBD. This is more prominent for Crohn’s disease than ulcerative colitis, with half of identical twins being concordant for Crohn’s. Extraluminal manifestations such as arthropathy, gritty red eyes or liver abnormalities are common.
2. Smoking is positively associated with Crohn’s and negatively associated with ulcerative colitis
Smokers are three times more likely to develop Crohn’s disease than non-smokers, but are half as likely to develop ulcerative colitis. The reasons for the differential effects of smoking remain poorly understood. Ulcerative colitis patients will often present for the first time or relapse on stopping smoking, whereas giving up smoking in Crohn’s has the highest odds ratio of any treatment for maintaining remission.
3. Faecal calprotectin can distinguish IBD from irritable bowel syndrome (IBS)
Crohn’s disease is much more difficult to diagnose than ulcerative colitis as symptoms are often non-specific and similar to many presentations of IBS. Faecal calprotectin assays have a 96% negative predictive value for excluding organic intestinal disease, including IBD. Faecal calprotectin is recommended by NICE for primary care use in distinguishing IBD from IBS1 and has been judged cost-effective at £22.79 per patient, compared with colonoscopy at £741.68 per person.
4. Ensure stool samples are sent to rule out an infective cause for patients with persistent diarrhoea
A stool sample for microscopy and culture is essential for all patients with persistent diarrhoea.
Stool samples are also key for patients with known IBD, as it is difficult to justify treatment with steroids or immunosuppression without first excluding an infective exacerbation.
5. Successful management of IBD needs to be multidisciplinary – don’t be afraid to ask for help early
The majority of patients with IBD have mild-to-moderate relapsing disease and do not require immunological therapies. The aim of management in primary care is to maintain remission, respond promptly to relapses and seek advice where necessary. All hospitals should now have a specialist IBD nurse who is available to contact for advice, support or to expedite urgent appointments to see a consultant.2 National IBD standards now recommend that all relapsing patients should be able to see a specialist within seven days of referral.
6. Aminosalicylates can prevent relapse and treat flares in ulcerative colitis
Mesalazine can reduce the risk of relapse in ulcerative colitis by more than 50%. In mild-to-moderate flares, escalating to a high dose will settle symptoms in most patients within two weeks. Consider topical 5-ASA therapy with suppositories for proctitis or foam enemas for distal disease. If there is no response at 14 days, consider a reducing regime of steroids, but co-prescribe calcium and vitamin D – this applies to all IBD patients requiring steroids.
Branded 5-ASAs should not be switched for generic preparations as they are highly specialised drugs and switching can result in disease relapse.
7. Crohn’s disease symptoms may be due to active inflammation or complications
5-ASAs are less effective in maintaining remission or treating flares in Crohn’s. For a mild-to-moderate flare, especially with perianal disease, consider adding antibiotics (metronidazole) as first-line escalation with a reducing regime of steroids as second line.
However, be cautious, as steroid treatment can sometimes mask underlying complications such as stenosing or fistulating disease.
8. Patients should be encouraged and supported in self-management3
Studies have shown that patients trained in self-management have quicker treatment, fewer hospital visits, reduced GP consultations and greater satisfaction with care than those with traditional management. Encourage patients to alter their medication dose according to their symptoms.
9. Surgery should not always be considered the last resort
A surgical option should always be considered for ulcerative colitis patients who have an acute flare or ongoing symptoms that are resistant to escalating medical therapy.
For patients with Crohn’s disease, medical therapy should be maximised and, in general, surgery avoided unless for complex disease with complications.
10. Patients with IBD have a higher risk of cancer
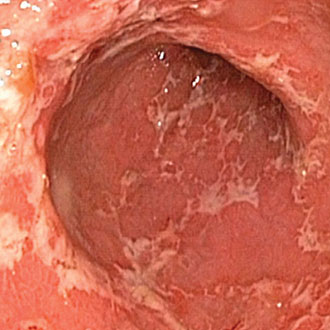
IBD patients with colonic involvement (both Crohn’s and ulcerative colitis) have an increased risk of colorectal cancer. Surveillance should start after eight years and the interval (one, three or five years) is then determined by the findings at colonoscopy.
Surveillance intervals need to be shorter if there is co-existent primary sclerosing cholangitis, family history or the presence of polyps. There is evidence that regular mesalazine reduces the increased risk of bowel cancer associated with colitis.
Dr Adam Haycock is a consultant gastroenterologist at The London Clinic and St Mark’s Hospital, Harrow
References
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









