Six top tips on improving mental health support for children and young people


In the next in our series showcasing highlights from our Pulse365 Live and Virtual events, Dr Amina Al-Yassin provides six key takeaway points for GPs on improving support for children and young people’s mental health – including what to do while waiting for CAMHS
There has been a palpable, and quantified, rise in the prevalence of mental health problems amongst children and young people particularly since the Covid-19 pandemic. 83% of GPs say they now see more young patients with mental health difficulties than they did in 2019, yet over half reported the majority of their referrals to CAMHS are rejected. Waiting times are variable, and can be long, with an average of 170 days, and 10% waiting for more than two years.
The following tips offer advice on what GPs can do to assess and support the children and young people who do not meet CAMHS thresholds or who are awaiting CAMHS support.
1. Ensure access for children and young people
With many GP surgeries moving to e-consultation first or triage first approaches, there is a risk that children and young people are unable to book in appointments or are barred by the online software from doing so owing to their age (Parents or guardians need to complete eConsults for children aged 6 months up to 16 years of age). Ensure that your surgery has mechanisms in place to allow adolescents to book themselves in if needed. If you do see an adolescent with their parent or carer, also give them an opportunity to speak to you alone. Mental health can be a sensitive subject and so it is important that any obstacles to accessing care are removed.
2. Make the initial assessment count
Assessment tools such as HEEADDSSS (Home, Education and Employment, Eating, Activities, Drugs, Suicidality, Safety) to get a holistic understanding of the CYPs life and TRAM (Transient, Reactive, Appropriate, Manageable) to differentiate between normal teenage angst and mental health concerns are useful. The key factors to elucidate in any mental health history are the severity, risk and functional impact of the condition as these will be key in deciding the course of action to take. Additionally, incorporating a mental state examination and, in specific presentations such as eating disorders, a thorough physical examination, are crucial components of the assessment process.
3. Recognise not everyone will need CAMHS
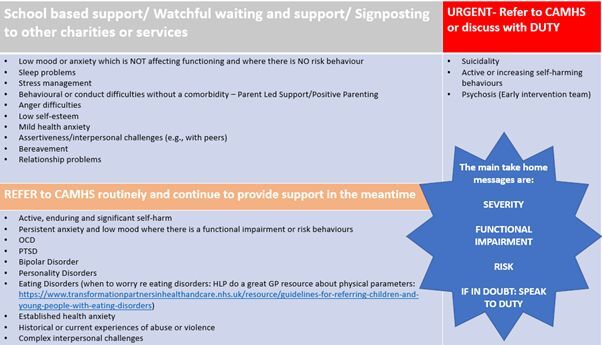
Determining which cases warrant referral to Child and Adolescent Mental Health Services (CAMHS) involves careful consideration of key factors, including severity, risk, and functional impairment. While some presentations (such as suicidality, active self harm and psychosis) may necessitate urgent intervention from specialist services, others may be managed effectively within primary care settings, schools, or in the VCSE sector (voluntary, community and social enterprises) with appropriate support and interventions.
GPs play a pivotal role in discerning the most suitable course of action based on the individual needs and circumstances of the child or young person and the following is provided as a guide only:
4. Optimise your CAMHS referral
Effective referral to CAMHS requires a comprehensive description of the child’s difficulties, functional impairments, and associated risks. Providing detailed descriptions, any collaborating reports from school, family or other professionals involved and including your mental state examination findings will ensure timely access to appropriate interventions. We recommend that the following are included in your referrals (see box):
Box: Checklist for optimising your CAMHS referrals
- Detailed description of the difficulties and how long they have been present
- What functional impairments or difficulties is this causing? (Eg, school attendance). Consider a HEADSSS assessment
- A brief mental state examination – please speak to the child directly (and ideally face to face) for this. This adds very helpful information which enables us to triage the referral more effectively
- A risk assessment – risk to themselves (suicide, self harm risk), to others and from others
5. Support children and young people awaiting CAMHS support
For children and young people who do not meet CAMHS criteria or are awaiting specialist support, primary care professionals play a crucial role in providing interim support and signposting to alternative services. The following website provide searchable databases of local and national mental health services:
- Footsteps Youth Wellbeing – Useful resources https://footstepsteesside.co.uk/services/useful-resources/
- Home – HappyMaps: Help and Resources for Children’s Mental Health
- For children and young people | Anna Freud
Equipping children and their families with self-help skills and techniques, such as grounding, distraction and coping strategies, providing useful learning resources such as Self Help Leaflets – Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (ntw.nhs.uk) and ensuring a safety plan is in place where appropriate empowers them to manage their mental health more effectively during the waiting period. Regular follow-up appointments and proactive monitoring enable healthcare professionals to address evolving needs and intervene promptly if the clinical picture changes.
6. Make sure you include safety planning
Safety planning is an essential component of managing child mental health concerns, particularly in cases involving suicidal ideation or self-harm. Collaborating with children and their families to develop personalized safety plans, which outline triggers, coping strategies, support networks (both personal and professional), and crisis interventions, enhances safety and resilience during times of heightened risk. Safety planning templates may be found online and can be easily incorporated into text messaging services, so that the discussion can be followed up with a written plan to be referred to when needed.
The prevalence of mental health issues among children and young people continues to rise, exacerbated by the challenges brought about by the COVID-19 pandemic.
In summary, GPs have a key role in assessing and supporting children and young people through ensuring access, conducting assessments, optimising referrals, offering support to those on waiting lists and equipping them with self-help skills and safety plans.
However, the role of the GP is unique and goes much further than being a referrer and signposter. The importance of the uniquely placed, community based, compassionate care that can be provided by a GP cannot be understated. GPs are respected and trusted by so many children and young people and there is power in each word you say.
A heavy dose of listening and validation of the struggles will go a long way. This is important, but not easy, work and GPs should look out for their own mental health and that of their colleagues- the practitioner health service is priceless for anyone who is struggling with this Practitioner Health.
By Dr Amina Al-Yassin is a GPwSI in child and adolescent mental health at Barnardo’s mental health team, Brent CAMHS SPIN fellow, and member of the RCGP Adolescent health group
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.










