Non-Covid clinical crises: Temporal (giant cell) arteritis
Signs, symptoms, blood tests
Temporal arteritis (giant cell arteritis, or GCA) is an autoimmune disease of older people that causes headache, scalp tenderness, jaw claudication (jaw pain with chewing), fever, sweats or weight loss. There may be aches and pains in the neck and arms, and sometimes the legs. Occasionally patients may have a cough. On examination, a swollen, tender or nodular temporal artery may be felt on one or both sides of the head, and the pulse may be more difficult to feel in that artery. CRP and ESR are usually elevated. Transient monocular visual loss or double vision are worrying features, suggesting involvement of the blood supply to the eye. Treatment is with high-dose steroids.
A difficult diagnosis
GCA is a difficult diagnosis to make as the symptoms can appear one by one; urgent specialist assessment is advised, even in a covid-19 outbreak, since GCA is recognised as a medical emergency. This may be even more important in the current outbreak since patients might present late, with impending or actual visual loss. COVID-19 can also cause headache, so beware: COVID-19 and GCA can mimic each other. Don’t worry about GCA in the under-50s; and GCA is fairly rare in the under-55s. Do worry about GCA if there is jaw claudication (present in about 50% of GCA patients) or visual loss.
Referring to a specialist
Most hospitals will have some provision for specialist assessment, either face-to-face or by telemedicine. It is usually better to refer by phone: the patient may be offered an appointment within 24 hours and should always be seen within 3 working days. Patients with visual loss or double vision should be referred to ophthalmology (eye casualty) whereas those without visual manifestations should usually be referred to rheumatology, but check local arrangements.
Initial tests and treatment
If you think GCA is more likely than any other diagnosis (including COVID-19), you should immediately start prednisolone 40-60mg daily, pending specialist confirmation of diagnosis. Try and ensure blood is sent to the lab before starting steroids, if possible. The practicalities of getting urgent blood tests are difficult during the COVID-19 pandemic, and you may need to discuss with a specialist to help weigh up the risks of attending hospital for a blood test – especially out of hours – versus the risks of waiting for an urgent specialist review. Being on long-term, high-dose steroids has serious implications for patients in a global pandemic. A normal CRP makes GCA much less likely, and is very helpful in making the decision not to commit the patient for a year or more of oral steroids. Lymphopenia is rare in GCA and might instead point towards COVID-19. Lastly, GCA symptoms usually respond rapidly to steroids. If symptoms don’t respond within a week, then reconsider the diagnosis; by this time, they should have been reviewed by a specialist either by phone or face to face.
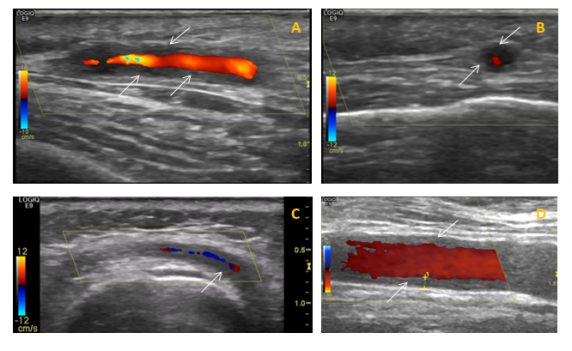
Biopsy and ultrasound tests
The diagnosis of GCA is usually confirmed by temporal artery biopsy; in some centres temporal artery ultrasound may be done as well as, or instead of, a biopsy. In the current outbreak, temporal artery biopsy may be unavailable; whether ultrasound is also available will depend on local arrangements. Ultrasound is best done within a few days of starting steroids.
Monitoring patients on high-dose steroids
Older patients taking high-dose steroids need to know they are extremely vulnerable to coronavirus, and should follow the government advice for the highest-risk individuals. High-dose steroids can cause depression, aggression or frank psychosis so a telephone follow-up to check on their mood is useful if they are socially isolated. Medical complications include diabetes and hypertension – if they have a home blood pressure monitor, encourage them to use it. Add a bisphosphonate, calcium and vitamin D to reduce fracture risk.
Tapering and relapse management
If the diagnosis of GCA is confirmed, after 4-6 weeks the steroid dose is tapered gradually over a year or more (see link below for dosing). During this time, make sure the patient knows who to contact if they have a relapse of GCA symptoms. Make sure they know to report jaw claudication urgently, even if they didn’t have this symptom at presentation, as this can be a precursor of visual loss. See the link below for steroid dosing at relapse, but if in doubt, seek specialist advice.
Further information for doctors and patients
The British Society for Rheumatology recently updated its clinical practice guidelines for GCA diagnosis and management[1]. The executive summary is free to read here. and includes checklists of symptoms, laboratory tests, how to taper steroids and how to manage relapses. For patients, there are patient-run support groups: PMRGCAuk and PMR GCA Scotland.
Dr Sarah L Mackie is associate clinical professor and honorary consultant rheumatologist at the University of Leeds and Leeds Teaching Hospitals NHS Trust
Ref
1. Mackie, S.L., et al., British Society for Rheumatology guideline on diagnosis and treatment of giant cell arteritis: executive summary. Rheumatology (Oxford), 2020.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









