
Case
Ms J is a 20-year-old student studying fine art who presents with a painful and discoloured right hand and wrist. She fell eight weeks ago playing netball and fractured her radius, and recently had her cast removed.
Her right hand and wrist are mottled and slightly swollen. The hand feels warm and she has intense pain over the dorsum. She cannot bear to be even lightly touched. The pain radiates up the forearm and her hand feels clumsy when she tries to move it.
You want to exclude infection or malunion, but also think this pain has neuropathic qualities and might even be complex regional pain syndrome (CRPS), previously known as reflex sympathetic dystrophy.
Problem
CRPS is usually post traumatic, following a radial fracture, for example. However, 10% of cases have no obvious causal event. CRPS is also usually unilateral, although in 7% of cases, additional limbs become involved. The incidence is similar to that of multiple sclerosis, but pain improves or even resolves within 18 months in 85% of cases. Half of these cases, however, persist, with long-term functional problems, and nearly half of patients do not return to work as a result of functional disability and residual pain.
Features
A CRPS limb has some of the following features:
• Pain disproportionate to any inciting event.
• Abnormal swelling.
• Abnormal colour, with the affected area appearing red, mottled or cyanosed, or all three at different times.
• Abnormal temperature, warm or cold.
• Abnormal sweating.
• Motor dysfunction, which can be a combination of pain-related dysfunction and motor dyspraxia.
• Abnormal skin or nail appearance.
Unusual symptoms, such as the feeling of limb dissociation, or altered sensory perceptions like limbs feeling longer (telescoping) or an abnormal shape, are common and should not be attributed to a psychological disorder.1 These symptoms are considered to be related to cortical changes, and altered two-point sensory discrimination can alert the clinician to this.
It is thought that central pain- processing mechanisms are important in the chronic sensitisation of the limb, and a limitation of movement and lack of normalising sensory input can perpetuate these mechanisms. It is also easy for painful limbs to become deconditioned, which may contribute to secondary causes of pain such as myofascial pain or hypomobile joints.2
Diagnosis
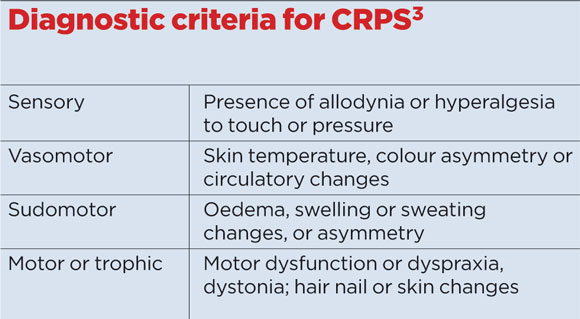
The diagnosis is a clinical one, but further tests are often indicated to exclude other pathology such as infection, inflammation, or malunion. At least two signs and three symptoms in the criteria listed below are considered diagnostic. To confirm the diagnosis it is usual to refer either to a pain specialist, or to another specialist such as an orthopaedic surgeon or rheumatologist.
Management
Pain intensity, disability, and distress are key areas requiring attention. Once other pathology has been excluded, mild CRPS may be managed in primary care. This includes those with mild to moderate pain and little disability and distress. CRPS inconsistent with this should be referred to a multiprofessional pain clinic as early as possible. Evidence suggests there is a window of opportunity for early treatments.
GP management will initially involve conventional medication such as anti-inflammatories, paracetamol, weak opioids or tramadol. If this fails, neuropathic medication should be titrated.
All those with CRPS should be encouraged to move the affected limb, although this may seem counterintuitive. Mild dysfunction may respond to simple advice and reassurance. Physiotherapists may also be involved, and advice should be focused on gentle movements. If significant dysfunction exists, it is important to involve physiotherapists or occupational therapists at an early stage.
Mild distress may be managed with reassurance and education, while more significant pain-related distress will require referral to a multiprofessional pain service for psychological treatment.
Other management includes steroids, bisphosphonates, autonomic nervous system blocks, and neuromodulation – all of which are usually considered in specialist pain clinics. UK guidance for the diagnosis, management and referral of CRPS, with clinician-specific sections, is available on the Royal College of Physicians’ website.3 This also includes useful information appendices.
Dr Chris Barker is a GP and clinical lead at Community Pain Service at Southport and Ormskirk Hospital NHS Trust, Merseyside
Dr Andreas Goebel is a consultant in pain medicine at The Walton Centre NHS Foundation Trust, Liverpool
References
1 Lewis JS, Kersten P, McCabe CS, McPherson KM, Blake DR. Body perception disturbance: a contribution to pain in complex regional pain syndrome (CRPS). Pain 2007;133:111-9.
2 Veldman PH, Reynen HM, Arntz IE et al. Signs and symptoms of reflex sympathetic
dystrophy: prospective study of 829 patients. Lancet 1993;342: 1012-6
3 Turner-Stokes L, Goebel A. Complex regional pain syndrome in adults: concise guidance. Clin Med 2011;11:596-600
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














