What not to do – musculoskeletal
Investigations
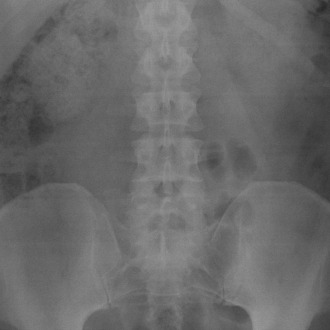
Do not offer X-ray of the lumbar spine for the management of non-specific low back pain1 –mechanical back pain is common and usually self-limiting within six weeks. Onward referral or physiotherapy is often not required for these patients, and investigation is not warranted as they will get better. Even in back pain that can be assumed to be caused by a prolapsed disc, or other identifiable pathologies, the spinal X-ray often does not show the site of the pain.
Discogenic pain and radiculopathy do not usually cause an abnormality on plain X-ray, and MRI scanning or CT scanning is required to demonstrate the abnormality. In addition, abnormalities on spinal X-rays are common and often bear no relation to the patient’s current pain. Degenerative changes are common over the age of 40 years, but are often symptomless and there is a poor correlation between abnormalities seen on X-ray and the patient’s problem.
Do not routinely measure bone mineral density (BMD) to assess fracture risk without prior assessment using FRAX (without a BMD value) or Qfracture – many factors influence the likelihood of the patient sustaining a fracture, such as their general mobility and the likelihood of them having a fall, and even patients with a normal BMD can sustain a fragility fracture (defined as a fracture sustained when falling from less than head-height in a patient over the age of 50 years). Therefore the FRAX database was established to enable clinicians to perform a fracture risk assessment, taking all the relevant risk factors into account, such as prior fracture, smoking status, inherited factors and other comorbidities such as rheumatoid arthritis. Qfracture is a similar database which was produced from the GP database.
Using Qfracture or FRAX enables the clinician to calculate a 10-year probability of the patient sustaining a major osteoporotic fracture and a hip fracture. If the 10-year probability of a major osteoporotic fracture is over 20% then preventative treatment is recommended (usually a bisphosphonate). If the risk is 10-20%, then a BMD measurement is generally recommended to aid calculation of the fracture risk. When using the FRAX tool, an individual patient risk can be plotted on a graph and the need to refer for BMD is represented graphically in three categories:
- high risk – treat the patient
- medium risk – perform BMD
- low risk – give advice and perhaps calcium/vitamin D supplements.
In patients over the age of 75 years, a DEXA scan is not required for QOF if they sustain a fragility fracture. Treatment can be started immediately as they are assumed to be suffering from osteoporosis.
Treatment
Referral for arthroscopic lavage and debridement should not be offered as part of treatment for osteoarthritis, unless the person has knee osteoarthritis with a clear history of mechanical locking (not morning joint stiffness, giving way or X-ray evidence of loose bodies)2 – arthroscopic lavage involves introducing fluid into the knee joint and washing out the joint. It was in vogue a few years ago to offer the patient an arthroscopic lavage (particularly in private medicine) if no other treatment was suitable. The evidence for this producing any benefit for the patient is unclear and a definite benefit has not been demonstrated, so NICE has said that it is not recommended.
In certain situations, arthroscopic examination is definitely recommended, and this is in the presence of loose bodies in the joint that have been demonstrated on X-ray or MRI and where these are thought to be causing locking of the joint. If meniscal degeneration has been demonstrated on MRI scan then the damaged meniscus can be removed arthroscopically.
The use of glucosamine or chondroitin products is not recommended for the treatment of osteoarthritis – glucosamine and chondroitin have been used empirically by patients suffering from joint pain for years. The evidence for their effectiveness has always been poor, but patients are willing to try anything when in pain and some do seem to derive benefit. The 2014 NICE OA guidelines looked at all the available evidence and found that there is a small benefit in knee OA from taking 1500mg of glucosamine sulphate as a single dose.2 There was no evidence that glucosamine chloride showed any benefit.
Unfortunately, glucosamine sulphate does not have a current medicines licence in the UK and cannot be prescribed, though the chloride formula is available. For this reason, the NICE guidelines group felt they could not recommend prescription of glucosamine, but suggested that patients bought the treatment themselves.
Rubefacients are not recommended for the treatment of osteoarthritis
However, topical NSAIDs and capsaicin gel have been shown to have short-term benefit for about four weeks when used for knee OA. The evidence for longer term treatment is lacking, but the revised NICE guidelines from 2014 still recommend them as an adjunct to core treatments for hand and knee osteoarthritis.
Topical NSAIDs have fewer side effects than oral NSAIDs and many patients do find them helpful.
Do not offer transcutaneous electrical nerve simulation (TENS) as a non-pharmacological therapy for low back pain – the NICE back pain guidelines (CG88 at www.nice.org.uk) explored the evidence for using TENS machines and found very little to show any benefit when compared with sham TENS treatments after a four week trial, and no economic benefit either.1
Referral
Do not delay referral of any person with suspected persistent synovitis of undetermined cause whose blood tests show a normal acute-phase response or negative rheumatoid factor3 – many patients are not referred promptly for specialist assessment when they present to their GP. The National Audit Office carried out an assessment of the treatment for people with rheumatoid arthritis in 2009 and found that approximately one third of patients delay presenting to their GP for more than three months when they develop symptoms of an inflammatory arthritis.4 In addition to this, GPs also delay referral and sometimes (in about 20% of patients) referral takes over a year from first presentation.
Some of the delay from primary care may be related to the fact that 10-20% of patients are seronegative for rheumatoid factor, yet still have active disease. GPs sometimes do not realise that negative serology does not rule out active joint inflammation. In addition, in the early phases of the disease when perhaps only a few small joints are affected, the ESR and CRP may still be low and only rise when the volume of inflamed synovium increases.
Therefore, when preparing the NICE guidelines, the guideline development group felt that it was important to ensure that patients with negative investigations and signs of inflammation are referred for assessment as soon as they present to their GP. There is a window of opportunity of about 12 weeks from onset of the disease, when the long-term outcome is much better if disease-modifying drugs are commenced within this time.5
Dr Louise Warburton is a GPSI in rheumatology and musculoskeletal medicine in Shropshire, and was a member of the NICE guideline development group for the rheumatoid arthritis guidelines.
References
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.











