How to spot zebras – recognising narcolepsy
What is it?
Narcolepsy is a long-term neurological disorder that causes, among other symptoms, a person suddenly to fall asleep at inappropriate times. It is caused by damage to the cells in the hypothalamus that excrete hypocretin, a neurotransmitter that regulates the sleep-wake cycle. The damage is thought to be autoimmune but can also occur after a brain injury. There are also occasional familial cases, which may be caused by hypocretin receptor problems.
Prevalence
The prevalence of narcolepsy worldwide varies from 0.03 to 0.16% of the general population, but it is estimated that there are many undiagnosed cases and a delay in diagnosis is also very common. Onset is most common around puberty but can occur at any age, with males and females equally affected. There was a rise in cases of narcolepsy in 2009/10 following the use of the Pandemrix swine flu vaccine, which is believed to have triggered an autoimmune reaction in some people.
Presentation
In narcolepsy, the brain is unable to regulate sleeping and waking patterns normally, which results in:
- Excessive daytime sleepiness – the person feels very drowsy throughout the day, has difficulty concentrating and staying awake, and has ‘micro-sleeps’ where they nod off momentarily and jerk awake again.
- Automatic behaviour – during brief sleeps the person will often carry on with the task they were performing without recollection of it later. This is almost certainly a symptom of sleep deprivation caused by fragmented night-time sleep.
- Cataplexy – temporary loss of muscle control resulting in weakness and possible collapse, often in response to strong emotions such as amusement (laughing) and anger. It can also happen as a response to pain. There is no loss of consciousness and the person retains full awareness of what is happening around them but is unable to speak or move voluntarily. Narcolepsy with cataplexy (about 60% of sufferers) is known as type 1 and narcolepsy without cataplexy is known as type 2.
- Sleep paralysis – experiencing a temporary inability to move or speak when waking or falling asleep, sometimes with terrifying nightmares.
- Excessive dreaming and waking frequently in the night – vivid (often ‘film-like’) and often terrifying dreams that come as the sufferer falls asleep (hypnogogic hallucinations) or just before or during waking (hypnopompic hallucinations).
- Falling asleep quickly but having difficulty maintaining sleep throughout the night leading, ironically, to overall sleep deprivation.
Narcolepsy doesn’t cause serious or long-term physical health problems but can have a significant impact on daily life and be difficult to cope with emotionally. It often coexists with anxiety and depression due to chronic sleep deprivation.
Problems with appetite and temperature control are also common.
At night, people with narcolepsy cannot achieve sufficient deep sleep with all its restorative properties. When they sleep, they fall quickly into REM sleep, which explains the vivid dreams and easy waking.
Differential diagnosis
Patients may be poor at explaining exactly what their symptoms are. They may simply present with tiredness and look like a typical ‘TATT’ (tired all the time) case, with difficulty sleeping at night. It’s easy to attribute this to psychosocial factors. They may present with episodes of cataplexy-related collapse, which can be mistaken for some kind of seizure or syncope.
Some points to consider in diagnosing narcolepsy are:
- Consider it as a possible differential when patients present with tiredness, insomnia or collapse. Ask questions that might reveal some of the associated features.
- Use the Epworth Sleepiness Scale – the score should be high in narcolepsy, with obstructive sleep apnoea (OSA) as a possible differential (in OSA there will be a clear history of snoring and interrupted breathing at night, with absence of the associated narcolepsy symptoms above).
- TATT blood tests should be normal, but a ferritin below 50 is a cause of increased periodic leg movements at night, which can easily wake a person with narcolepsy who is only ever sleeping lightly.
If you think narcolepsy is a possible differential you will need to refer. For adults, a sleep clinic is the best option, preferably one that has a consultant with a special interest in narcolepsy.
Even in sleep clinics, delayed or misdiagnosis is not uncommon as these clinics will have much more experience with OSA. For children, an acute paediatric or child development referral is needed as an intermediate step, as paediatric sleep clinics are usually tertiary referral centres.
Diagnosis
This essentially pivots on a careful history but is supported by specialist investigations:
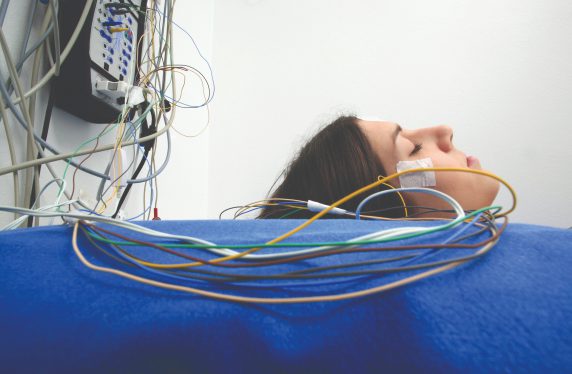
- Sleep studies overnight followed by daytime multiple sleep latency tests (a daytime nap where REM sleep is achieved quickly).
- Looking for the associated genetic markers – HLA DR2 or DQB1*0602 present in a high proportion of people with narcolepsy, although this is not in itself diagnostic.
- Measurement of CSF hypocretin levels via lumbar puncture. These levels are usually extremely low in narcolepsy, especially with cataplexy.
Follow-up
- Long-term specialist follow-up is recommended.
- Treatment for most people with narcolepsy will be a combination of planned sleep routines, lifestyle adjustments and drug therapy. It is important that a personalised approach to treatment is taken.
- CNS stimulants can be taken to promote daytime wakefulness. Methylphenidate, modafanil and lisdexamphetamine can be transformational for excessive daytime sleepiness. Most GPs should be able to access shared-care agreements for the prescribing of CNS stimulant drugs.
- Medications to promote night-time sleep: modified-release melatonin, iron and other restless leg treatments if restless leg syndrome is causing night-time waking. In cases of narcolepsy with cataplexy that continue to be problematic, there are orphan drugs that can be used at night – Xyrem (sodium oxybate) and pitolisant are very effective, very expensive, and are in the domain of the specialist prescriber.
- Associated depression, anxiety and appetite problems need to be addressed alongside the narcolepsy. The SSRI antidepressants, particularly fluoxetine and venlafaxine, are known to reduce the incidence and severity of cataplexy collapses, so are often the first choice in a person with narcolepsy.
CAMHS, adult mental health, IAPT and weight management services may need to add input to the overall package of care, but close liaison with a narcolepsy expert is essential to achieve the insights necessary to offer the best possible support to the patient.
People with narcolepsy will experience effects across all areas of their life. Personal relationships, school, work and social activities are all affected.
They will need to inform the DVLA and are likely to have their driving licence suspended until adequate control can be proven.
Patient support groups like Narcolepsy UK are invaluable sources of support, information and advocacy for sufferers and their loved ones. Find them at narcolepsy.org.uk/
Dr Amanda Molloy is a GP in Crawley, Sussex
Conflicts: none declared
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.











