Patient assessment
Do not suspect MS in patients with non-specific symptoms.
The same applies for trigeminal neuralgia, except if it is in an atypical context or if the patient is younger than 40 years.1 ‘Atypical’ or ‘mixed’ trigeminal neuralgia is when there is a persistent discomfort between paroxysms or sensory loss, and is more often refractory to treatment than classic trigeminal neuralgia.2
Do not diagnose epilepsy in those presenting with a transient loss of consciousness (TLoC) if the history is suggestive of an uncomplicated vasovagal syncope or of situational syncope.
Diagnose uncomplicated faint when there are no features to suggest an alternative diagnosis and there are any of the following features in the history suggestive of an uncomplicated faint – the three Ps:
• Posture – prolonged standing or similar episodes that have been prevented by lying down.
• Provoking factors – pain or a medical procedure.
• Prodromal symptoms – sweating or feeling hot before the loss of consciousness.
Diagnose situational syncope when there are no features to suggest an alternative diagnosis and syncope is clearly and consistently provoked by straining during micturation (usually while standing), or by coughing or swallowing.3
Do not diagnose cluster headache in the absence of autonomic features on the same side of the headache.
Autonomic features include:4
• Red or watery eye.
• Nasal congestion or runny nose.
• Swollen eyelid.
• Forehead and facial swelling.
• Constricted pupil or drooping eyelid.
Investigations
Do not investigate those with a typical migranous aura.
A typical aura involves visual symptoms, sensory symptoms or speech disturbance that develop gradually over at least five minutes, last up to 60 minutes and are fully reversible.4
Do not refer people diagnosed with tension-type headache, migraine or medication-overuse headache for neuroimaging solely for reassurance.5
Current evidence shows no significant reduction in anxiety, depression or fear of illness, or improvement in quality of life, in patients who underwent scanning, neither is there any clinical benefit. There can also be a significant amount of anxiety caused by incidental findings on scans.1
Do not routinely use EEG in the investigation of transient loss of consciousness (TLoC).
An EEG should not be performed in a case of probable syncope because of the possibility of a false-positive result. Brief seizure-like activity can occur during uncomplicated faints and is not necessarily diagnostic of epilepsy.6
An ECG is much more important when investigating TLoC in adults, unless there are clear seizure markers, such as post-ictal amnesia and confusion, or cheek or tongue biting.3
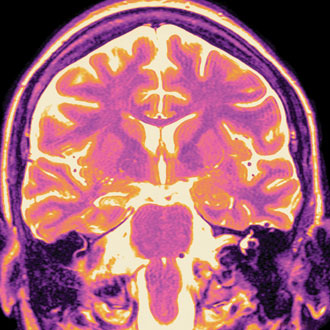
Do not arrange an MRI in general practice for those with optic neuritis or transverse myelitis (motor weakness, sensory disturbance with a sensory level, sphincter involvement), as these may be due to MS.
Refer immediately to a specialist who will investigate. Do not delay diagnosis, as early treatment can be beneficial for long-term prognosis, so it is important for GPs to identify patients with symptoms suggestive of MS.2
Treatment
Do not offer opioids for the treatment of tension-type headache.
Aspirin, paracetamol or NSAIDs should be used instead. Use of these 10 times per month or more leads to medication- overuse headache, so this risk should be discussed.5,7
Do not offer ergots or opioids for the acute treatment of migraine.
A combination treatment, with a triptan and paracetamol or a triptan and NSAID for migraine, should be offered ahead of monotherapy on the basis of clinical and cost-effectiveness evidence. Combination treatment was superior to monotherapy with aspirin, paracetamol, NSAIDs or triptans. If patients wish to take only one drug, then aspirin, paracetamol, an NSAID or triptan are recommended.
If one triptan is ineffective others may work, as lack of effectiveness is not a class effect.4,5
Do not offer paracetamol, NSAIDs, opioids, ergots or oral triptans for the acute treatment of cluster headache.
Oxygen, or subcutaneous or nasal sumitriptan, is recommended for the treatment of cluster headache. There is no evidence to support the use of opioids for any primary headache disorder. Opioids may cause medication-overuse headache and therefore should be avoided.4,5
Do not prescribe the progestogen- only pill (POP) in women taking enzyme-inducing antiepileptic drugs (AEDs).
The POP is not recommended as reliable contraception in women and girls taking enzyme-inducing AEDs. There is also a new recommendation in the 2012 NICE epilepsy guidance about the interaction between lamotrigine and oestrogen-based contraceptives, as this can result in a significant reduction in lamotrigine levels and may diminish seizure control.6
Do not discuss disease-modifying therapy (DMT) in depth with patients with MS, as this will be done in secondary care.
In particular, do not discuss when the patient has had a ‘clinically isolated syndrome’ (CIS) – in other words, a single episode – as they may expect treatment with DMT. However, the use of DMT after a CIS remains controversial.8 These arguments should be left for the neurology team to discuss with the patient rather than the GP, who is understandably unlikely to be as well versed in recent research.
Do not offer long-term treatment with steroids in patients with MS or advise them to use hyperbaric oxygen.
Research evidence does not show beneficial effects on the course of the condition with either long-term steroids or hyperbaric oxygen.8
Dr Estelle McFadden is a GPSI in neurology in Bradford, and a member of the executive council for the Primary Care Neurology Society
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens