Lifestyle medicine in primary care


In the latest in our series from Pulse Live talks, Dr Jo Fleming and Dr Hussain Al-Zubaidi discuss how to implement lifestyle medicine in primary care
As the ever-increasing burden of long-term health conditions continues to hit primary care, the need to prevent and reverse these conditions is becoming more urgent.
A lifestyle medicine approach aims to modify the behavioural and lifestyle bases of disease, rather than simply treating the disease1. It is defined by the British Society for Lifestyle Medicine (BSLM) as ‘an evidence-based discipline, which supports patients to prevent, manage and reverse certain chronic conditions, using supported behaviour changes skills and techniques to create, and sustain lifestyle changes’.
Lifestyle medicine requires the patient to be an active partner in the process rather than a passive recipient of medical care1. In the conventional model of primary care, with GPs having 10-minute consultations to treat a particular ailment, the idea of implementing this approach might seem difficult or unachievable.
However, primary care has evolved. Primary Care Networks (PCNs) offer increased potential for change. The services delivered by PCNs were designed to support the goals of the NHS Long Term Plan, including improving population health, increasing collaboration between practices and supporting the integration of primary care with other parts of the health and care system.
The Additional Roles Reimbursement Scheme (ARRS) provides funding to create bespoke multi-disciplinary teams. PCNs can assess the needs of their local population, and employ social prescribers, health and wellbeing coaches, dieticians and pharmacists. These roles can be used to great effect to implement lifestyle medicine in primary care.
Example: Leamington Spa Primary Care Network
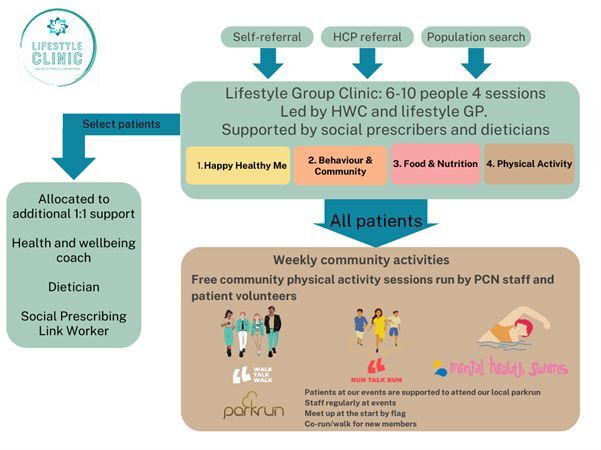
Dr Hussain Al-Zubaidi, a lifestyle GP in Leamington PCN, set up a lifestyle clinic for patients across Leamington North and Leamington South PCN in 2020. Two lifestyle clinics run each week, with support from additional primary care ARRS staff and physical activity groups.
Selected patients can access one-to-one ongoing support from social prescribers, dieticians and a health and wellbeing coach. Figure 1 (below) shows the patient journey for a Leamington PCN patient wanting support with their lifestyle.
Figure 1
What does a group lifestyle clinic look like?
Groups are run twice a week in two GP practices; one in evenings, and one in mid-mornings. This offers different locations and times of the day to increase patient accessibility. The groups include six to 10 patients from all eight practices in Leamington PCN. There are four sessions.
1: Happy, Healthy Me: a general overview and reflection of what being healthy and happy means to each individual, and what areas of wellness they feel they would like to improve. Patients are asked to complete a food diary.
2: Behaviour Change and Community: what is behaviour, can we change it and what are the barriers? The power of community in adopting new behaviours.
3: Food and Nutrition: what food does for our bodies, what a good diet looks like, reflections on how we eat / food diary discussions.
4: Physical Activity: what has happened to physical activity, how much physical activity should we be doing and what counts, reflections on what physical activity we enjoy / used to enjoy and what some of the barriers might be to taking part; opportunities to be physically active in the local community.
What do patients need?
Successful patient contacts require engagement, education and evolution. Applying the model above can help to achieve these.
Engagement – the patient needs to feel listened to. The group setting of lifestyle clinics can help, with patients being given a platform where they can speak and share experiences.
Education – there often is not enough time in a GP consultation to educate about lifestyle. The lifestyle clinics offer education from the health professional running it, but an important focus is for patients to engage in discussion and reflection, and learn from the experiences of others.
Evolution – patients need support in making changes. Group lifestyle clinics can give patients an entry point into this, while also offering further continuous community groups for maintenance, such as walking and swimming groups. By providing these additional activities we build a foundation for our patients to support what we discuss in the clinics. Patients who attend all four lifestyle clinic sessions are also, if appropriate, able to access up to six one-to-one health coaching sessions over a period of six months. These give them the opportunity to explore their situation and create new insights. The health and wellbeing coach facilitates and supports behaviour changes that the patient may not have been able to achieve alone.
Case study
Linda lives with obesity. She has become anxious about going out due to her size, and has low mood. Referred by her GP, she attends all four lifestyle clinic sessions, learns some new information and enjoys meeting other patients in a similar situation. She feels less alone and starts to make some initial changes.
When contacted by the health and wellbeing coach a few weeks after the clinic, Linda says she still wants to change, but she faces barriers including a busy family life. She knows what she should be doing, but can’t seem to implement it. Linda is offered one-to-one health coaching. She wants to address her weight – she doesn’t feel ready to tackle food, but is keen to include physical activity into her life. Walking is too difficult but swimming appeals.
However, the idea of going to our PCN Swim Together group at a public pool is too daunting. Through health coaching sessions, Linda is able to address the barriers preventing her from going swimming. Over time, Linda addresses these and eventually feels ready to attend one of our PCN Swim Together sessions. She enjoys it and starts investigating other aquatic activities she can do at the leisure centre.
Linda now feels that physical activity is becoming more established in her life, something which she didn’t previously think was possible. She has gained confidence and is ready to tackle other aspects of her lifestyle, including food. Further health coaching sessions facilitate this, and if and when Linda feels ready, our dietician is also ready to offer advice and support in conjunction with the health coach to support her.
It’s not just about the patients
While addressing the needs of our patients is a priority, so too are the health and wellbeing of our primary care staff. Primary care staff are often reaching levels of burn out and their own physical and mental health is suffering2.
The Active Practice Charter can help in improving staff health as well as that of their patients. GP practices can sign up to the Active Charter, and receive Active Charter status by achieving five simple, self-declared criteria:
Reduction in sedentary behaviour in staff
Further information can be found on the RCGP Physical Activity Hub.
A further initiative to help both staff and patients is the parkrun practice initiative. Established in 2018, this is a RCGP collaboration with parkrun UK to promote the health and wellbeing of staff and patients. GPs and other staff members of general practice value the importance of teamwork for boosting their morale and mitigating burnout3. Where staff from parkrun practices have engaged in parkrun practice activities there have been positive effects on morale and participation4.
GP practices across the UK are encouraged to develop close links with their local parkrun to become parkrun practices. You can get in touch with your local parkrun via the parkrun map, register your GP practice on the parkrun practice website and access a parkrun practice toolkit with lots of ideas as to what a GP practice can do.
How to convince a PCN to invest
- Build a business case for using ARRS roles in this way. You will need the expertise of health and wellbeing coaches, dieticians, social prescribers, and care coordinators to deliver a robust lifestyle service.
- Highlight the benefits of group clinics in terms of economies of scale, staff development, and patient engagement.
- Start small. Look for quick, low-cost wins, through ideas set in the Active Practice Charter and parkrun practice toolkit. This can help change the culture within the PCN and put you in a better position in the future to develop more advanced projects like this.
- Seek external funding for additional setting up costs of groups, e.g. local councils, active partnerships and sport legacy funding.
- Measure outcomes against PCN Key Performance indicators, to show how what is being implemented is helping patients and the PCN achieve targets.
We need to look beyond purely treating disease, much of which is driven by factors such as environment, social deprivation, unhealthy consumption patterns and lifestyles, and instead look towards prevention and maintenance of good health in our patients and staff. Through primary care teamwork and PCN collaboration, implementation of interventions such as these can start to shift this model of care to one centred on wellness and doing our bit to combat the obesogenic environment.
References
- Egger G, Binns A, Rossner S, Sagner M. Introduction to the Role of Lifestyle Factors in Medicine. Lifestyle Medicine: Lifestyle, the Environment and Preventive Medicine in Health and Disease, chapter 1, 3-13, 2017.
- Hall LH, Johnson J, Watt I, O’Connor DB. Association of GP wellbeing and burnout with patient safety in the UK primary care: a cross sectional survey. British Journal of General Practice, 2019. Link
- Galetta-Williams H, Esmail A, Grigorolou C et al. The importance of teamwork climate for preventing burnout in UK general practices. European Journal of Public Health, volume 30, issue supplement 4, iv36–iv38, 2020. Link
- Fleming J, Bryce C, Parsons J, Wellington C, Dale J. Engagement with and delivery of the ‘parkrun practice initiative’ in general practice: a mixed methods study. 2020.

Pulse 365 LIVE Events cover a broad array of topics pertinent to you, your patients, and your practice. You will gain free CPD and be able to take part in live Q&As. Specifically created for all practising, GMC-registered GPs and trainees, you will hear from experts across primary and secondary care, and network with like-minded GPs. Sign up for your nearest event today.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.
Related Articles
READERS' COMMENTS [1]
Please note, only GPs are permitted to add comments to articles











Using a digital approach at scale we are getting just over 50% of a T2DM population into remission. 70% have improved glycaemic control and are in a better metabolic place.
A CD said “there is no drug that can do this.
We agree, the new verb is this is “foodable”
My work is now a place of utter joy.