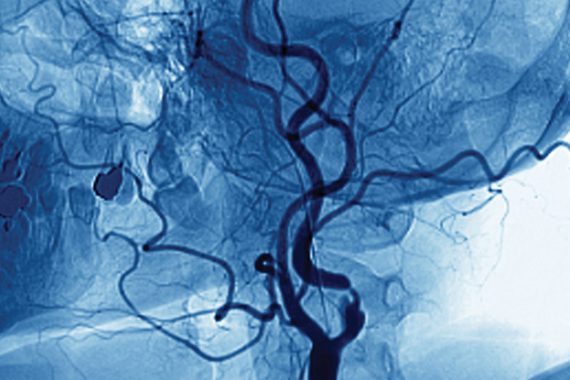
1 Improving cancer survival
The good news story on cancer has undoubtedly been the improvement in survival rates.
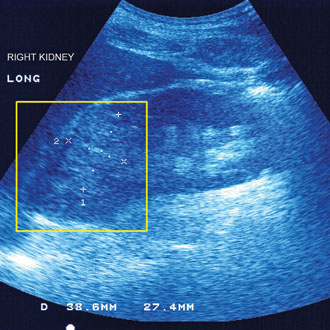
kidney cancer sonography spl 330x330px SUO
Over the past decade, the gap between UK and similar European countries has narrowed and – although the reasons behind this are complex – experts are quick to point to the impact of GPs’ work on earlier diagnosis.
Cancers are increasingly being detected through GP urgent referrals, while fewer are being diagnosed as emergencies.[1] Increased use of the two-week wait urgent referral pathway is tied to improved survival.[2]
Professor Willie Hamilton, professor of primary care diagnostics at the University of Exeter, says this ‘strongly suggests it’s the GP bit that has made a major contribution’ to better outcomes.
He adds: ‘While we GPs have been doing more referrals and more tests – it’s paying off. Lives are being saved.’
Dr Ishani Patel, GP clinical lead for the Transforming Cancer Services Team, London, says GPs have upped their game ‘through audits, cancer significant event analyses and cancer profiles data’.
2 Controlling antibiotic prescribing
Reading the national newspapers may give a different impression, but GPs have led the way in reducing unnecessary use of antibiotics.
General practice is the one area of the health service where antibiotic use is now steadily falling year on year, with a cut in overall antibiotics prescribing of 7% in the past year. The most recent Public Health England surveillance report from 2015 showed total GP antibiotic prescriptions decreased by more than 4% between 2011 and 2014, whereas hospital outpatient prescriptions went up by 9% and inpatient prescriptions by 12%.[3]
GPC clinical and prescribing subcommittee chair Dr Andrew Green says the reduction is ‘remarkable’ and ‘a testament to GPs who have invested enormous effort into the slow process of educating patients’.
Indeed, the reduction may come at a cost for practices; a recent study showed those that prescribe fewer antibiotics are less likely to score well in the GP Patient Survey.[4] And GP experts say it remains unclear how far GPs can continue to cut antibiotic use without missing serious infections. A recent study showed practices that achieved substantial reductions did see a small increase in complications, although these were largely treatable.[5]
3 Reducing CVD mortality
The rate of cardiovascular disease deaths has fallen by three-quarters since 1961, and GPs have played a crucial part.
More than half this reduction is a result of changes in population risk factors – principally smoking cessation, and also better control of blood pressure and cholesterol by general practice.[6] The substantial decline in the incidence of vascular dementia over the past two years has also been attributed to much better risk factor management in primary care.[7]
Professor Mike Kirby, visiting professor at the Faculty of Health and Human Sciences, University of Hertfordshire, highlighted the important role of GP practices, saying there was no doubt the improvement ‘is partially due to better management of risk factors and appropriate prescribing – well done, primary care’.
4 Cutting the burden of infant GI infections
The introduction of the oral rotavirus vaccine in 2013 into an already crowded immunisation schedule for infants was always going to be a challenge.
Despite this, GPs have achieved around 90% coverage for both doses of the vaccine, with enormous benefits. Official figures indicate some 90,000 infections were prevented in the first year, with a 60% drop in cases – an improvement that was sustained last year.[8]
Professor Anthony Harnden, professor of primary care at the University of Oxford and GP advisor on the Joint Committee on Vaccination and Immunisation, says: ‘Rotavirus diarrhoea is a significant burden for infants, parents, nurseries, hospitals and GPs. Fortunately, with the high vaccination coverage GPs have achieved, there has been a significant reduction in recent laboratory reports of rotavirus.’
5 Eradicating Hib infection
GPs will see hardly any cases of invasive Haemophilus influenzae type B (Hib) disease these days, and the eradication of this devastating illness is due to immunisation by the profession.
After GPs started delivering the Hib vaccination programme in 1992, the number of cases of invasive Hib disease fell dramatically over the following six years, from nearly 900 per year to fewer than 50 in 1998. There were signs of resurgence in the early 2000s, but the introduction of the fourth booster in 2004 has almost completely eradicated the disease in infants.[9]
As Professor Harnden says: ‘I remember the alarming experience of my first night on call as a senior house officer in paediatrics in 1985, seeing a young child at 3am with acute Haemophilus influenzae epiglottis struggling to breathe.
‘Invasive Hib is now very rare – there was only one reported case in the under-five age group in 2015.’
6 Bringing down the rate of teenage pregnancies
The rate of teenage pregnancies was only going up – until GPs were tasked with improving access to long-acting contraception. In 2009, QOF indicators were introduced and soon after NICE reported a large increase in prescribing of implants.

teenage pregnancy almy 330x330px SUO
Research shows that conception and abortion rates among under-18s fell dramatically between 1998 and 2011 – both linked with increased LARC usage.[10] A recent Lancet report showed teenage pregnancies were at a record low, at fewer than 25 conceptions per 1,000 women aged 15–17 in 2013.[11]
Dr Anne Connolly, GPSI in gynaecology and chair of the Primary Care Women’s Health Forum, says: ‘We know it made a difference when more GPs were funded and trained to do more long-acting reversible contraception, because it increased choice and access to more reliable methods.’
But she warns recent public health cuts may set this progress back. She says: ‘Without those skills women may end up going back to more old-fashioned, user-dependent methods of pills or condoms, or nothing.’
7 Promoting evidence-based medicine
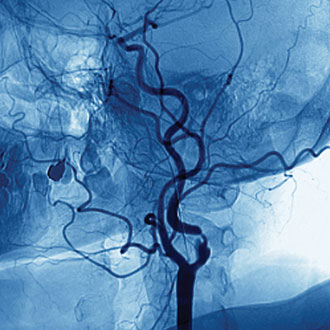
narrowed neck artery angiogram spl 330x330px SUO
GPs have become the champions of evidence-based medicine in the NHS, while keeping the emphasis on treating patients as individuals.
The introduction of NICE in 1999 and the QOF in 2004 brought an avalanche of new guidance and incentives for GPs, some good, others more questionable.[12] GPs have been able to take the best of this new rational approach to medicine and blend it with their strong sense of holism.
As Professor Martin Marshall, a GP in east London and professor of healthcare improvement at University College London, says: ‘Dramatic improvements in compliance with evidence-based guidelines in practices have been seen where I work in east London resulting from the QOF’.
But he adds that ‘some of the gains are harder won, requiring GPs to ignore or bypass their narrow contractual obligations and do what their professional conscience dictates is right, sometimes irrespective of the personal consequences’.
Dr Martin Duerden, RCGP prescribing advisor, says a shift in patient demographics and the pressure to use drugs to prevent disease has also ‘put intense pressure on GPs’. But he says: ‘What has impressed me is that despite these pressures and inadequate funding, general practice has adjusted to these needs and in many cases has been able to continue to provide holistic, personal care.’
8 Cost-effective prescribing
GPs have saved the health service £7bn over the past 40 years by prescribing generics.[13] This has allowed 490 million more items to be prescribed with no increase in spend. The UK now has an 84% primary care generic prescribing rate – among the highest in the world.
Although this may not improve care for individual patients, it does allow resources that would otherwise be lost to the NHS to be used in other ways.
Dr Andrew Green says prescribing is now ‘more rational and consistent between practices’ and that GPs are ‘far more willing to share their prescribing patterns’ and learn from colleagues.
Medicines management teams and better software have helped, and some GP practices have worked closely with pharmacists and nurses within their own teams to optimise prescribing.
But Dr Green cautions that arbitrary attempts to ration local prescribing by some CCGs are ‘contrary to NHS rules and prevent individualised care’.
9 Coping with rising multimorbidity
It’s an oft-quoted statistic that GPs deal with roughly 90% of all patient contacts with the NHS – even more impressive when you consider the complexity of their patients has been rising steadily, at the same time as their slice of the total health budget has been shrinking.
GPs ‘multitask and deliver high-quality care whatever presents to us’, former RCGP chair Professor Clare Gerada says. And Department of Health figures confirm that multimorbidity is rising,[14] with half of people over the age of 50 living with two or more long-term conditions in 2012.[15]
GPs could be forgiven if they had passed the buck to their specialist colleagues – but their unique skills in managing risk and advocating the best approach for each patient have seen them continue to absorb the large burden of contacts without recourse to secondary care.
Dr John Cosgrove, RCGP Council member and a GP in Birmingham, says GPs ‘take pride in referring and prescribing only when absolutely necessary’ even though the ‘only incentive for this is professional pride and a hope of reducing future anxiety’.
10 Improving diabetes care
With so many stark warnings about the impending diabetes epidemic, it is easy to forget just how far management of diabetes has come over the past two decades.

pregnany woman, pregnancy – online
Much of this progress has been made by GPs. Data on QOF measures show a consistent improvement in the control of patients’ glucose, blood pressure and cholesterol levels – in line with NICE-recommended care for the prevention of serious complications, such as retinopathy and kidney disease.[16]
Dr Roger Gadsby, associate clinical professor at the University of Warwick and GP clinical lead for the National Diabetes Audit, says the work of GPs to improve risk factor control has ‘had a powerful effect’. He adds: ‘If you give GPs good evidence and good resources, they will deliver.’
References
1. National Cancer Intelligence Network Short Report – Routes to Diagnosis 2006-2013, preliminary results. http://www.ncin.org.uk/view?rid=3026
2. Møller H et al. Use of the English urgent referral pathway for suspected cancer and mortality in patients with cancer: cohort study. BMJ 2015; 351: h5102 http://www.bmj.com/content/351/bmj.h5102
3. Public Health England – English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) 2010 to 2014. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/477962/ESPAUR_Report_2015.pdf
4. Ashworth M et al. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pr 2015; published online 7 December http://bjgp.org/content/early/2015/12/04/bjgp15X688105
5. Gulliford M et al. Safety of reduced antibiotic prescribing for self-limiting respiratory tract infections in primary care: cohort study using electronic health records. BMJ 2016;354:i3410 http://www.bmj.com/content/354/bmj.i3410
6. Unal B et al. Explaining the Decline in Coronary Heart Disease Mortality in England and Wales Between 1981 and 2000. Circulation 2004; 109 (9):1101-1107 http://circ.ahajournals.org/content/109/9/1101
7. Jagger C et al. A comparison of health expectancies over two decades in England: results of the Cognitive Function and Ageing Study I and II. Lancet 2015; 387: 779-786 http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)00947-2/abstract
8. Public Health England – Infection Report 9 (30): 28 August 2015 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/457925/hpr3015_rtvrs.pdf?
9. Public Health England – Infection report 10 (8): 26 February 2016 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/503792/hpr0816_hib.pdf
10. Connolly et al. Association between long-acting reversible contraceptive use, teenage pregnancy, and abortion rates in England. Int J Womens Health 2014; 2014: 961-974 https://www.dovepress.com/association-between-long-acting-reversible-contraceptive-use-teenage-p-peer-reviewed-article-IJWH
11. Wellings K et al. Changes in conceptions in women younger than 18 years and the circumstances of young mothers in England in 2000–12: an observational study. Lancet 2016; published online 23 May http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30449-4/abstract
12. Campbell et al. Quality of primary care in England with the introduction of pay for performance. NEJM 2007; 357:181-190 http://www.nejm.org/doi/full/10.1056/NEJMsr065990
13. The King’s Fund – Better value in the NHS. http://www.kingsfund.org.uk/publications/better-value-nhs
14. Department of Health – Long-term conditions compendium of information – Third edition: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf
15. Barnett K et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380: 37–43 http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(12)60240-2.pdf
16. Calvert M et al. Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009; 338:b1870 http://www.bmj.com/content/338/bmj.b1870
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens