Case 1
Mr P is 70 years old and has a BMI of 35. He has a history of ischaemic heart disease, hypertension and is a smoker. The GP is called to see him because he is complaining of a sudden-onset, severe, right-loin-to-groin pain.
He is rolling about the bed unable to get comfortable, and examination is difficult. The GP diagnoses renal colic, administers rectal diclofenac and arranges to phone in one hour to check on progress. Before then, the patient deteriorates and his wife calls an ambulance. At A&E, he is diagnosed with a ruptured abdominal aortic aneurysm and transferred to surgery.
GP’s diagnosis
Renal colic.
Actual diagnosis
Leaking abdominal aortic aneurysm.
Clues
The patient was older than average for a case of renal colic and was known to be an arteriopath.
Take-home message
Severe back or loin pain in an older arteriopath is a leaking aneurysm until proven otherwise.
Case 2
Mr H, a 73-year-old former smoker, presents with a three-month history of deteriorating urinary symptoms – variable urinary flow, frequency and nocturia. Abdominal examination is unremarkable. Digital rectal examination (DRE) reveals a moderately enlarged, benign-feeling prostate. The GP counsels the patient and organises a PSA test. Tamsulosin is prescribed and the patient is asked to return in three months. After four weeks there is no improvement. Mr H is referred to urology and found to have non-visible haematuria. Flexible cystoscopy shows velvety erythematous areas on the trigone of the bladder. General anaesthetic cystoscopy confirms carcinoma and he is started on intravesical BCG.
GP’s diagnosis
Lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia.
Actual diagnosis
Carcinoma in situ of the bladder.
Clues
Approximately 20% of patients with bladder cancer or carcinoma in situ have irritative voiding symptoms. Visible or non-visible haematuria will be a feature in the vast majority.
Take-home message
All patients presenting with LUTS should have urinalysis.
Case 3
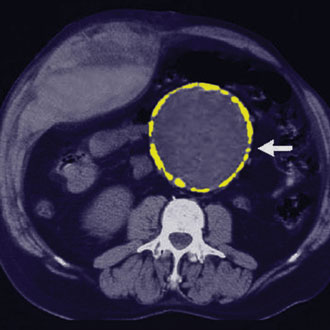
Mr M is a 65-year-old construction worker with a history of hypertension. He presents with a four-week history of constant lower back pain, and thinks it may have started after lifting masonry, but cannot be sure. It is stopping him sleeping and affecting his ability to work. Neurological examination is normal, as is his straight leg raise. He has significant paravertebral tenderness and muscular spasm, so he is diagnosed with mechanical back pain, given NSAIDs and antispasmodics, and told to rest.
Initially, the analgesics help and he returns to work. Six weeks later his legs ‘give way’. In hospital, an MRI finds multiple metastatic deposits in his spine, causing cord compression. His PSA is >1000 and he has a hard nodular prostate on DRE. He is started on steroids and urgently seen by oncology.
GP’s diagnosis
Mechanical lower back pain.
Actual diagnosis
Metastatic carcinoma of the prostate leading to spinal cord compression.
Clues
The age of the patient and nature of the pain should make you consider other differentials. Although there is weak evidence to support traditional ‘red flag’ symptoms prompting investigation1, each case should be evaluated on its merits and repeat examination considered.
Take-home message
In older men with unexplained lower back pain, assess the prostate.
Professor Abhay Rane is a consultant urological surgeon at Surrey and Sussex Healthcare NHS Trust
Mr James Henderson is a specialty doctor in urology at Surrey and Sussex Healthcare NHS Trust
References
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens