Case
You see 63 year old man who has, in recent months, noticed a few episodes of haematospermia. Genital and rectal examinations are normal, his urinalysis reveals no abnormality and a PSA is within normal limits. As the symptom continues, you refer him to the urology department, where he has a cystoscopy and transrectal ultrasound of prostate and seminal vesicles. You receive a letter from the urologist stating, ‘No cause found for haematospermia, reassured and returned to your care.’ But the patient is actually far from reassured when he sees you to discuss the situation, and says, ‘There must be something wrong.’
Where do you go from here? How can he be managed going forward? What other assessment or investigation might be appropriate?
The problem
Haematospermia is a distressing symptom for patients, however despite investigation a cause is not found in as up to as many as 70% of patients, most cases being self-limiting.1 In this case physical examination, dipstick urinalysis, DRE and PSA testing are the correct initial investigations to be performed in primary care. The patient was then correctly referred to urology as per NICE guidelines2 (see table 1). The thorough set of investigations performed here will have looked into any obvious causes. However despite this, if symptoms persist and the patient is still concerned, further urological and non-urological investigations are available.
In the above case the key questions to be answered are:
- Is any further urological investigation warranted?
- Is there any non-urological investigation indicated?
- What is the patient’s primary concern?
The most important thing is to stress to the patient that the symptom is most likely benign and self-limiting, he was appropriately investigated and there is a high chance that further investigation will not find a cause. Obviously though, he was not reassured in clinic.
Table 1 – NICE Criteria for referral to urology in patients presenting with heamatospermia2
| Indications for referral |
|---|
|
All men aged over 40 years with no identifiable cause for haematospermia found in primary care |
|
Men of any age with signs and symptoms suggestive of prostate cancer |
|
Men and boys of any age who have experienced more than ten episodes of haematospermia, with no identifiable cause found in primary care |
|
Men and boys where initial investigations have suggested that the underlying cause of haematospermia may be cysts or calculi of the prostate or seminal vesicles |
|
Men and boys who continue to experience haematospermia despite treatment of a suspected underlying cause identified in primary care |
Management in primary care
Ruling out the differentials
If a cause is to be found for persistent haematospermia, the majority (50%) are due to infection and of those patients who undergo secondary care investigations, the rate of malignancy is reassuringly low, from 2-5.6%.3,4 Other causes that can be investigated include duct obstruction, cysts, vascular abnormalities, trauma (in particular trauma that may occur to the prostate or penis during sex) and systemic causes.5 There is also the phenomena of pseudo-haematospermia which should be considered; the suction of partner’s blood into the urethra during sex1, a symptom which could be picked up on history-taking in the urology clinic.
History, including a sexual history, should be retaken and assumptions should not be made based on the patient’s age. Trauma is an important cause of haematospermia5 and embarrassing conversations about prostatic stimulation and sexual practices should not be avoided or assumed to have been done at the urology outpatient clinic. If this reveals no new information, further investigation could be performed.
In general practice a few basics can be done first to rule out systemic causes of haematospermia. The simplest way to do this is to rule out severe hypertension by checking blood pressure and organising some basic blood tests to check platelets and clotting, to ensure no bleeding abnormality exists.
Infection should be the next cause to be investigated. Prostatovesiculitis and posterior urethritis can present with haematospermia in up to 55% of patients,6 therefore inflammatory markers and urinary culture should be considered (it is important to remember that urinalysis is not 100% sensitive).7 A travel history should also be taken to determine the risk of urinary tuberculosis or schistosomiasis.1 These rarer infections can be diagnosed by urinary microscopy and bladder biopsy respectively, re-referral at this point may be appropriate if haematuria is present on dipstick or the patient has travel history to high risk countries.8
In the above case, the prostate and bladder have been imaged – this is usually indicated by the presence of haematuria. Cystoscopy served to exclude malignancy of the urethra and bladder. However no mention of imaging of the testicles has been mentioned. Testicular cancer is less likely in the older male; however there is a second smaller peak of incidence in older males9, therefore testicular examination should be performed and if there are concerns, an ultrasound should be considered.
The patient’s primary concern, given his age, may well be prostatic cancer and when taking a history risk factors should be assessed. If his symptoms persist, despite the normal PSA and DRE, further investigation could be considered (combined PSA and DRE will only pick up about 95% of cancers).10 If at this point the patient’s symptoms have persisted and no further cause has been found, further investigation may be appropriate. This would need to be organised via secondary care so re-referral would be required, including details of the normal investigations performed in primary care.
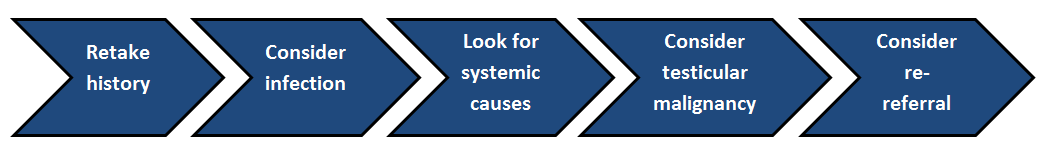
Figure 1 – Approach to persistent haematospermia following normal initial investigations
Further investigations
The question of what urological investigation should be performed next is not an easy one, given the normal investigations so far and the patient’s currents symptoms. MRI is probably the next useful test11, it could not only be helpful for detecting prostatic cancer (sensitivity quoted as ranging from 60% to 96%12) but it is also helpful in detecting the more likely benign causes (prostatic/peri-prostatic cysts or prostatic calculi13,14). If an abnormality is detected, targeted biopsy would be required to then confirm the diagnosis.
Transrectal ultrasound-guided biopsy of the prostate would require justification, perhaps based on the MRI. It is worth noting that biopsy in itself is a common cause of haematospermia.4 These risks should be discussed with the patient prior to any invasive procedure being performed, however the benefits of a negative biopsy for patient reassurance in light of a raised PSA, MRI findings or palpable mass shouldn’t be underestimated.
Ongoing management
If there is no cause found for the haematospermia despite the intensive investigations now performed, treatment options are limited. Finasteride has been investigated as an option for symptomatic treatment but there are insufficient numbers in the study describing this to prove statistical benefit. There are risks of impotence with the finasteride that detract from regular use of this drug in this setting. Other studies describe the use of a course of anti-inflammatory medications15 however also lack statistical significance. Blind use of antibiotics should not be encouraged.
For those patients with refractory haematospermia whose symptoms continue to cause distress, referral to a sub-specialist in andrology may be required. Transurethral resection of the ejaculatory ducts is one treatment option for the patient, however more recent studies from the Asian Journal of Andrology indicates Holmium laser incision via a ureteroscope confers lower recurrence rates.15
In summary, this is a difficult situation and the symptoms may persist despite treatment. It is most likely a benign condition and despite extensive investigation a cause may not be found. In all cases, good communication skills, sensible safety netting and appropriate investigations will help reassure the patient that it is unlikely that their main concern, likely to be cancer, is responsible.
Dr William Fowler is a core surgical trainee in urology at the Freeman Hospital, Newcastle.
Dr Rakesh Heer is a senior lecturer at Newcastle University and an honorary consultant urologist at the Freeman Hospital, Newcastle.
References
- Waseem Akhter Should every patient with haematospermia be investigated? A critical review. Cent European J Urol. 2013; 66(1): 79–82.
- Management of a person with haematospermia – NICE – https://cks.nice.org.uk/haematospermia#!scenario
- Weidner W, Recurrent haemospermia–underlying urogenital anomalies and efficacy of imaging procedures Br J Urol. 1991 Mar;67(3):317-23
- Michael J. Mathers, PD Dr. Haematospermia—a Symptom With Many Possible Causes Dtsch Arztebl Int. 2017 Mar; 114(11): 186–191.
- Haematospermia – A Systematic Review Priya Kumar. Ann R Coll Surg Engl. 2006 Jul; 88(4): 339–342
- Ahmad I, Krishna NS. Hemospermia. J Urol. 2007;177:1613–1618.
- Jeff A. Somerville et al. urinalysis – a comprehensive review.
- Darren J Gray Diagnosis and management of schistosomiasis. BMJ. 2011; 342: d2651
- Michael J. Garner . Epidemiology of testicular cancer: An overview Volume116, Issue3 1 September 2005 Pages 331-33
- William J Catalona Comparison of percent free PSA, PSA density, and age-specific PSA cutoffs for prostate cancer detection and staging Urology Volume 56, Issue 2, August 2000 , Pages 255-260.
- Imran Ahmad Hemospermia – review article. The Journal of urology. May 2007 Page: 1613-1618
- Alexander P.S.Kirkham How Good is MRI at Detecting and Characterising Cancer within the Prostate European Urology Volume 50, Issue 6, December 2006 , Pages 1163-1175
- V G McDermot Prostatic and periprostatic cysts: findings on MR imaging American Journal of Roentgenology. 1995;164: 123-127
- In R.Cho Magnetic Resonance Imaging in Hemospermia. The Journal of Urology Volume 157, Issue 1, January 1997 , Pages 258-262
- Xiao-Jun Wu Clinical outcome of treating intractable haematospermia using holmium laser incision through a ureteroscope Asian J Androl. 2016 Jan-Feb; 18(1): 140–142
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














