Rational referrals: Urology
Consultant surgeon and professor of urology Professor Rakesh Heer, specialist urology registrar Mr Subhabrata Mukherjee and consultant urologist Miss Eva Bolton advise on how to navigate referral pathways for urological conditions
Advice and guidance
Renal cysts found coincidentally on scans
Simple renal cysts incidentally found on ultrasound or CT scan generally do not need any treatment or follow-up unless patients are symptomatic (for example, with pain or infection), in which case a routine urology referral should be made. However, complex renal cysts (such as cysts with septations or a soft tissue component) may be renal cancer and need an urgent two-week-wait referral.
Renal stones found coincidentally on scanning
Kidney stones without hydronephrosis are often asymptomatic. Patients should have blood tests checking a renal profile, bone profile and uric acid. Small (≤4mm) non-obstructing renal stones can be managed conservatively in the community with fluid and diet advice11 and follow-up imaging in six to 12 months’ time.
Large staghorn stones may damage renal function, so consider an urgent referral. Patients with a kidney stone at the PUJ causing hydronephrosis should be treated like ureteric colic and referred to a same-day acute surgical or urological unit or A&E. They probably need urgent renal decompression or expedited stone operation. Patients with renal stones should be warned the stone may drop in the ureter and block urine drainage from the kidney, which leads to sudden onset flank pain (ureteric colic). If so, the patient should go to A&E.
Cases requiring same-day referral
Ureteric colic
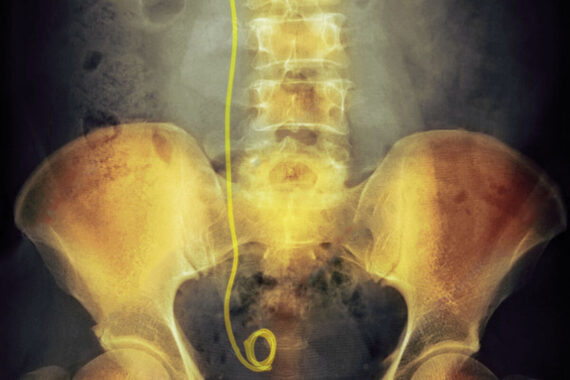
Patients with suspected ureteric colic should be referred to a same-day acute surgical unit or A&E.1 A large audit looking at the CT scan reports of nearly 1,000 patients attending A&E with suspected ureteric colic showed that the chance of finding a ureteric stone is around 40%. Of the remaining patients, 40% had a normal scan and 20% had non-stone related pathologies that were urological (pyelonephritis, pelvi-ureteric junction [PUJ] obstruction, renal cyst), or non-urological (appendicitis, diverticulitis, mesenteric panniculitis, adnexal mass).2 Patients with ureteric colic will generally get a CT scan in A&E and be referred to the appropriate specialty after the scan finding. If a patient with an obstructing ureteric or PUJ stone develops infection, it becomes a potentially life-threatening urological condition and needs urgent decompression of the kidney by means of a ureteric stent or nephrostomy.3
Suspected testicular torsion
Testicular torsion is an acute urological emergency and needs urgent scrotal exploration.4 It is a time-sensitive diagnosis as a delay at this stage decreases the testicular salvage rate.5 If a testicular torsion is suspected, the patient should be referred urgently to the nearest same-day acute surgical unit or A&E for the attention of the urologist. If there is any doubt, refer urgently on the same day.
Visible haematuria
Patients with visible haematuria with large clots, clot retention or haemodynamic instability should be referred to A&E as they are likely to need an urgent three-way catheter insertion, bladder wash, irrigation and possibly a blood transfusion.
Mostly, haematuria settles down in a day or two. The haematuria work-up, which involves cystoscopy to assess the bladder and a CT urogram to assess the upper urinary tract, is usually done as an outpatient. However, if haematuria persists, the patient may be taken to theatre for cystoscopy under anaesthesia and a bladder wash. Patients with mild to moderate visible haematuria, stable vital signs and normal haemoglobin levels should be referred on the urgent, two-week-wait pathway for investigations.
Urgent, two-week-wait referrals
NICE describes the symptoms, signs and investigations6 that trigger a urological cancer referral via the two-week wait pathway.7,8
Suspected prostate cancer
If the prostate feels malignant on digital rectal examination or PSA levels are above the age-specific reference range:
• Below age 40 Use clinical judgment, considering family history and black ethnicity.
- Age 40–49 PSA more than 2.5µg/l.
- Age 50–59 PSA more than 3.5µg/l.
- Age 60–69 PSA more than 4.5µg/l.
- Age 70–79 PSA more than 6.5µg/l.
- Age above 79 Use clinical judgment.
Suspected bladder cancer
Aged 45 years and over with:
- Unexplained visible haematuria without UTI.
- Or visible haematuria that persists or recurs after successful treatment of UTI.
Aged 60 years and over with unexplained non-visible haematuria and either dysuria or a raised white cell count on a blood test.
Suspected renal cancer
- Unexplained visible haematuria without UTI, clots, retention or instability.
- Or visible haematuria that persists or recurs after successful treatment of UTI.
Suspected testicular cancer
- A non-painful enlargement or change in shape or texture of the testis.
Suspected penile cancer
- A penile mass or ulcerated lesion, where an STI has been excluded as a cause or a persistent penile lesion after treatment for a sexually transmitted infection has been completed.
Cases requiring routine referral
Acute urinary retention discharged from hospital with catheter
If the patient is discharged from A&E or urology with a catheter following an episode of acute urinary retention, the follow-up plan should be stated in the discharge summary. In general, if it is the first episode of retention due to enlarged prostate, the patient is started on an alpha-blocker and an outpatient trial without catheter (TWOC) is arranged in seven to 10 days by the hospital. If TWOC is unsuccessful, the patient may need bladder outlet surgery, a long-term catheter or intermittent self-catheterisation. There is a long waiting list for bladder outlet surgery. The long-term catheter needs to be changed in the community, every eight to 12 weeks.
Chronic urinary retention
Patients with chronic urinary retention9 characterised by gradual development of the inability to empty the bladder completely should have an urgent blood test checking renal profile and electrolytes and an urgent ultrasound scan of the urinary tract. If renal function and electrolytes are normal and there is no hydronephrosis, the patient can be referred to urology routinely.
However, if there are signs of high-pressure chronic retention, meaning backpressure from the bladder retention up to the kidneys, characterised by impaired renal function or bilateral hydronephrosis, the patient should be referred to a same-day acute surgical or urological unit or A&E. Presence of nocturnal enuresis, a non-tender palpable bladder and treatment-resistant hypertension may also point to high-pressure chronic retention.10
Patients with low-pressure chronic retention with a high residual urine volume (over about 400ml) should also see the urologist sooner rather than later as there is a risk that the condition may turn into high-pressure chronic retention causing renal impairment.
Patients with a history suggestive of ureteric colic seen after the episode
Only 40% of suspected cases of ureteric colic are shown to have a stone on scanning.2 If the patient already had a scan in the A&E, it is important to check the formal report and act accordingly as a preliminary report may be issued out of hours. However, if the patient did not have a CT scan and the colic has subsided, it is advisable to get an ultrasound scan of the whole abdomen and rule out hydronephrosis from an obstructed stone or any other obvious abdominal pathology. Even a normal ultrasound scan may warrant a CT scan to look for other causes, on a case-by-case basis.
Recurrent proven UTIs in adults
Recurrent UTI in adults is defined as two or more documented UTIs in the last six months or three or more in the last 12 months.12 NICE recommends non-urgent referral for people aged 60 and over with recurrent or persistent unexplained UTI.7
Indications for urgent urology referral are frank haematuria (refer by the two-week-wait pathway), neurological disease (such as spinal cord injury, spina bifida), pneumaturia, faecaluria, proteus on repeat urine cultures, suspected urinary stone, obstructive symptoms or structural or functional abnormality13 and pregnancy, after discussion with the obstetrics team.14
Pneumaturia
Pneumaturia may result from an entero-vesical fistula, recent urinary tract instrumentation, catheterisation or (rarely) emphysematous cystitis. Persistent pneumaturia without recent instrumentation or catheterisation should prompt an urgent urology referral.
Unexplained chronic testicular pain
Differential diagnoses of chronic testicular pain include chronic epididymitis, epididymal cyst, spermatocele, hydrocele and varicocele. Sometimes pain can be neurogenic or even idiopathic.15 Arrange an ultrasound scan in the community and if there is no suspicion of testicular cancer, make a routine referral. If you suspect testicular cancer, refer under the urgent two-week-wait pathway.
Mr Subhabrata Mukherjee is a specialist registrar in urology, Miss Eva Bolton is a consultant urologist, and Professor Rakesh Heer is chair of urology, all at Imperial College London, Charing Cross Hospital, Imperial College Healthcare NHS Trust
References
- Gandhi A, Hashemzehi T, Batura D. The management of acute renal colic. Br J Hosp Med 2019;80:C2–6
- Mukherjee S et al. “Pseudo-renal colic” – a neglected common entity with significant impact on health service providers’ resources during both pre-and peri Covid-19 pandemic. European Urology 2021: S349-S349
- Hinojosa-Gonzalez D, Torres-Martinez M, Villegas-De Leon S et al. Emergent urinary decompression in acute stone-related urinary obstruction: a systematic review and meta-analysis. J Clinical Urology 2023;16:19-31
- Laher A, Ragavan S, Mehta P et al. Testicular torsion in the emergency room: a review of detection and management strategies. Open Access Emerg Med 2023;12:237
- Howe A, Vasudevan V, Kongnyuy M et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol 2023;6:1159-66
- NICE. Clinical knowledge summary: symptoms suggestive of urological cancers. 2021
- NICE. Clinical knowledge summary: referral for suspected urological cancer. 2021
- NICE. Clinical knowledge summary: urological cancers – recognition and referral 2021
- BNF. Treatment summary: urinary retention
- Madhushankha M, Jayarajah U, Kuruppu C et al. Clinical characteristics and outcome of high-pressure chronic urinary retention: a systematic review. J Clin Urol 2023;15:204-12
- British Association of Urological Surgeons 2023. Information about your condition
- NICE. Urinary tract infection (recurrent): antimicrobial prescribing. 2018. NG112
- Khor V, Aslim E, Ng L et al. “Pop goes the whistle” – noisy micturition as the main presentation of pneumaturia. Urol Case Rep 2019; 23:106-7
- Patient. Guidelines for Recurrent Urinary Tract Infections in Adults: Antibiotic Prophylaxis Definition of Recurrent Lower Urinary Tract Infection
- Leslie S, Sajjad H, Siref L. Chronic testicular pain and orchalgia. StatPearls Publishing 2023
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









