Dr Shammy Noor explains the latest evidence-based approach to chronic kidney disease (CKD) management, including how to prescribe newly recommended treatments
Pharmacological management of CKD is dependent on a number of variables, each with a different focus on patient outcomes. The mainstay of management is still to control cardiovascular risk and limit disease progression. This includes intensive management of blood pressure and coexisting conditions.
New in the arena are sodium-glucose cotransporter-2 (SGLT2) inhibitors and potassium binders.
SGLT2 inhibitors lower blood sugar levels by preventing the kidneys reabsorbing glucose, thereby increasing urinary glucose. They have shown significant benefit in clinical trials in type 2 diabetes. In the latest NICE guidelines for type 2 diabetes, they are now considered first line, alongside metformin, for many patients.1
In addition to their anti-diabetes qualities, SGLT2 inhibitors have shown significant promise in cardiovascular outcomes in patients with CKD, and NICE now recommends SGLT2 inhibitors for some patients who do not have diabetes.
Before initiating treatment, it is fundamental to assess the patient for CKD.
GPs are familiar with the use of eGFR for assessment of kidney function, with a persistent (longer than three months) drop in eGFR below 60ml/min/1.73m2 indicating a CKD diagnosis. However, it is less well established that urinary ACR (uACR) is also key to the diagnosis of CKD and in determining the best therapeutic option. NICE recommends using both eGFR and uACR to determine the presence and level of risk associated with CKD.2 For example, patients can be at high risk even with normal, category G1 eGFR (above 90mg/ml/1.73m2) if they are in category A3 uACR (above 30mg/mmol).
CKD management – general advice
- Assess for and manage risk factors and co-morbidities of CKD.
- Be vigilant with (or avoid) nephrotoxic drugs that cause AKI (especially during intercurrent illness) – most commonly NSAIDs but also several classes of antibiotics, such as gentamicin and vancomycin.
- Manage associated anxiety or depression.
- Reduce risk of CVD.
- Offer lifestyle and diet advice.
Statins
NICE recommends offering atorvastatin 20mg for primary or secondary prevention of CVD to people with CKD. CKD is a major independent risk factor for CVD.
Look for a 40% reduction in non‑HDL cholesterol and increase the statin dose to achieve this. But consult a nephrologist before increasing the dose if the eGFR is below 30ml/min/1.73m2.
Hypertension management
Blood pressure control is fundamental in the management of CKD. Before starting antihypertensive treatment, ask yourself:
- Is the patient diabetic?
- What is the level of proteinuria (measured using uACR)?
NICE recommends treatment to a target blood pressure of below 140/90mmHg in those with uACR below 70mg/mmol, and below 130/80mmHg in those with uACR above 70mg/mmol.2
If hypertension remains uncontrolled after four antihypertensive drugs at therapeutic doses, refer to nephrology.
Renin-angiotensin-aldosterone system (RAAS) inhibitors and hyperkalaemia
A key issue in the use of ACE inhibitors or ARBs is the monitoring of eGFR and potassium. NICE advises:2
- Measure U&E before starting. Repeat between one and two weeks after starting and after each dose increase.
- An eGFR decrease less than 25% (from baseline) or a creatinine rise of less than 30% (from baseline) does not require dose adjustment.
- Do not routinely offer if the pre-treatment potassium is greater than 5.0mmol/l.
- Stop if potassium increases to 6.0mmol/l (once other hyperkalaemic medicines have been discontinued).
- Potassium binders may be of use (see below).
Potassium binders
NICE has approved two drugs – sodium zirconium cyclosilicate and patiromer3,4 as an option for:
- Emergency care for acute life-threatening hyperkalaemia (secondary care only).
- For people with category G (formerly stage 3b to 5) CKD
– who need a RAAS inhibitor but get persistent hyperkalaemia when taking it
– are not on dialysis.
If the patient is consistently getting high potassium levels after starting an ACE inhibitor or ARB (above 6.0mmol/l), sodium zirconium cyclosilicate or patiromer can be used to bind and stabilise serum potassium. This then allows the patient to continue on the very useful RAAS antagonist with the hyperkalaemia risk mitigated.
These drugs are available to primary and secondary care. Currently, for the most part, they are initiated in secondary care and the prescribing continues in primary care. See your local guidelines for more information.
SGLT2 inhibitors
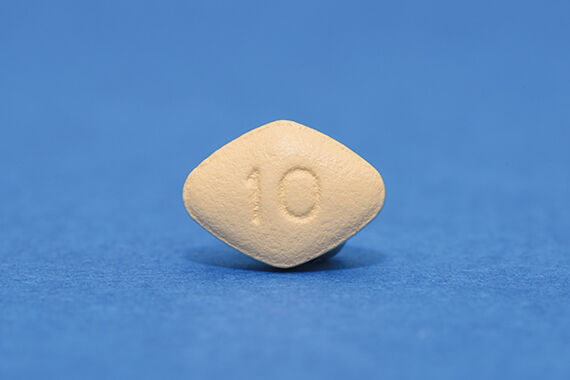
These medications have a unique mechanism of action, lowering glucose independent of insulin. In type 2 diabetes, SGLT2 inhibitors have become quickly established. They currently include dapagliflozin, canagliflozin, empagliflozin and ertugliflozin.
The use of SGLT2 inhibitors in diabetes is covered in NICE NG28.1 Note they are not suitable for patients with type 1 diabetes.
Dapagliflozin is currently the only SGLT2 inhibitor with a NICE technology appraisal to be used in patients without diabetes in CKD.5
For CKD, again ask yourself two questions:
- Is the patient diabetic (type 2 only)?
- What is the level of proteinuria (as measured by uACR)?
Follow the steps in Table 1.
Table 1: Prescribing recommendations for SGLT2 inhibitors according to proteinuria and diabetes status
| Urinary ACR | Patients without diabetes | Type 2 diabetes patients |
| A1 (<3mg/mmol) | SGLT2 inhibitor not indicated | Use SGLT2 inhibitor in line with NG28 recommendation for glycaemic control2 |
| A2 (3-30mg/mmol) | SGLT2 inhibitor not indicated unless uACR >22.5mg/mmol – dapagliflozin recommended | Use a maximised ACE inhibitor or ARB Consider adding an SGLT2i |
| A3 (>30mg/mmol) | Use a maximised ACE inhibitor or ARB Dapagliflozin recommended | Use a maximised ACE inhibitor or ARB Offer an SGLT2 inhibitor with ACE inhibitor/ARB |
SGLT2 inhibitors and low eGFR
A peculiarity of this drug class is that its glycaemic benefit is highly dependent on active renal function. It becomes less efficacious for diabetes glucose control once the eGFR drops below 60ml/min/1.73m2. If the SGLT2 inhibitor is being used solely for type 2 diabetes, it is generally not recommended for initiation below an eGFR of 45ml/min/1.73m2. If the SGLT2 is being used for CKD (or for heart failure), it can still be used at lower eGFRs. The advice on this is frequently changing and it can be different for each of the available SGLT2 inhibitors, so you should check the latest guidance for that particular drug.
SGLT2 inhibitor prescribing considerations
Diabetic ketoacidosis (DKA)
A major consideration is the risk of DKA, which is a potential serious side effect of SGLT2 inhibitors. The following criteria should be followed:
- Do not use in Type 1 diabetes in primary care.
- Check to see if they have ever had DKA and be very cautious if they have.
- Check if they are following a very low carbohydrate or ketogenic diet – this should be suspended before initiating SGLT2 inhibitors.
You should counsel the patient about DKA, its presentation (especially if the patient has an intercurrent illness – see sick day rules) and to ensure the patient seeks medical help if this occurs.
Sick day rules
DKA risk increases significantly when the patient is unwell and unable to eat and drink as usual – this advice could prevent DKA.
- Diarrhoea and vomiting or fever – stop SGLT2 inhibitors and don’t restart until eating and drinking fluids normally for at least 24 hours.
- Stay hydrated with water (or sugar-free fluid).
- Have a lower threshold to seek medical advice if unwell with infection or illness.
- Stop SGLT2 inhibitors prior to surgery (take advice from pre-op clinic).
Common adverse effects
SGLT2 inhibitors increase the passage of glucose into the urine and this is a main cause of many of the side-effects, which include:
- Increased risk of UTI and vulvovaginitis (including candida infections).
- Volume depletion and polyuria effects (polydipsia, postural hypotension, dehydration).
- Although SGLTs do not cause hypoglycaemia, the concurrent use of insulin or sulfonylureas can increase hypoglycaemic risk.
- Less common adverse effects include DKA.
- Uncommon – Fournier’s gangrene.
For common minor infections refer to your local guidelines for management. However, for patients with a very high risk of UTIs or genital infections, such as perineal gangrene, including those with recurrent and neurological bladder conditions, SGLT2 inhibitors are probably not advisable.6
Monitoring
Check renal function before initiating treatment and at least annually thereafter. Keep an eye on the latest advice for individual SGLT2 inhibitor drugs if the eGFR drops below 60mg/ml/1.73m2.
Dr Shammy Noor is a medical author, GP partner and trainer in Lichfield, Staffordshire, and UK medical director for the digital healthcare company Healthy.io
References
- NICE. Type 2 diabetes in adults: management. NG28 updated 2022.
- NICE. Chronic kidney disease: assessment and management. NG203. 2021
- NICE Technology appraisal guidance TA599. Sodium zirconium cyclosilicate for treating hyperkalaemia. 2019
- NICE Technology appraisal guidance TA623. Patiromer for treating hyperkalaemia. 2020
- NICE Technology appraisal guidance TA775. Dapagliflozin for treating chronic kidney disease. 2022
- Yang H, Choi E, Park E et al. Risk of genital and urinary tract infections associated with SGLT-2 inhibitors as an add-on therapy to metformin in patients with type 2 diabetes mellitus: A retrospective cohort study in Korea. Pharmacol Res Perspect 2022;10:e00910
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens