Ten top tips – pulmonary hypertension
1. Look out for pulmonary hypertension
Pulmonary hypertension (PH) is defined as a mean pressure of more than 25mmHg in the pulmonary artery. Echocardiography is used to screen patients and a formal diagnosis is made at cardiac catheterisation. There are 7,000 people in the UK living with PH. If it is left untreated, PH leads to death within three years. Treatments are not curative, but can improve patients’ quality of life.
2. Be aware of the causes
- Left heart failure (the commonest cause, seen typically in older people with impaired left ventricle function, who are on diuretics, ACE inhibitors or ß-blockers).
- COPD.
- Connective tissue disease.
- Congenital heart disease.
- Chronic thromboembolic disease (for instance, after DVT).
- Obstructive sleep apnoea, with or without obesity or hypothyroidism.
- Idiopathic or genetic (rare).
3. Know what to look for in the history
- Breathlessness on exercise.
- Syncope, sudden collapses or near-syncope.
- Short history – often only a few months.
- Reduced exercise ability.
- Problems swallowing if scleroderma.
- A smoking history.
- Use of illicit or slimming drugs such as amphetamines.
- Family history of sudden early death.
4. Know what you’ll find on examination
- Cyanosis.
- Finger clubbing.
- Right heart failure (see point 6).
- Scleroderma, with tight finger skin, hair loss, ulcers on the fingers and tight red shiny skin around the mouth if connective tissue disease is the cause.
5. Know which tests might be needed
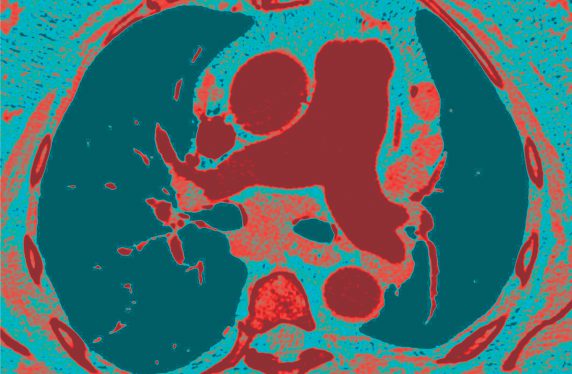
- Chest X-ray, looking for a large heart and enlargement of pulmonary arteries and disproportionately small peripheral vessels.
- ECG – looking for right ventricular hypertrophy (tall R waves and downwards T waves in lead V1).
- BNP (elevated in any patient with PH).
- Echocardiogram.
6. Exclude left heart disease as a cause
Left heart disease (stiff left ventricle causing PH) is more likely if the patient is obese, hypertensive or diabetic. You can manage this using standard treatment for left heart disease – a rehabilitation programme with exercise, weight loss, diuretics, ACE inhibitors and blood pressure medication. An echocardiogram will support the diagnosis by reporting LV systolic or diastolic dysfunction.
If the patient has signs of right heart failure (ascites, ankle oedema, raised JVP) this could be due to a failing left ventricle but might be the result of pulmonary arterial hypertension (PAH). This will need urgent treatment.
7. Refer urgently if you suspect PAH
Refer to your local pulmonary hypertension clinic or to the cardiology or respiratory team nearest to the patient’s home. The patient should be seen within two weeks.
8. PAH medication will be started in secondary care
PAH will be managed by the pulmonary hypertension team, who will start appropriate medication such as sildenafil or tadalafil. The other treatments are endothelin receptor antagonists (ambrisentan, bosentan, macitentan) or prostanoids (intravenous epoprostenol).
9. Be aware of medication side-effects
Sildenafil causes nasal congestion, increased nosebleeds and acid reflux. These can be managed symptomatically.
Endothelin receptor antagonists can cause liver dysfunction, so patients need liver function checked every few weeks. It is important to maintain iron levels, normal thyroid function, appropriate calorie intake and gentle exercise.
10. Be prepared to refer to palliative care
PH is a life-limiting disease. Survival depends on the underlying diagnosis but may be as short as a few months or as long as several years. If there is rapid progression, the pulmonary hypertension service will refer the patient to palliative care or lung transplantation.
Professor Robert Tulloh is a professor of congenital cardiology and pulmonary hypertension at the Bristol Heart Institute. Dr Louise Tulloh is a GP at Helios Medical Centre, Bristol.
Conflicts: none declared
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









