What to do with lung nodules
Presentation
Pulmonary nodules are defined as focal lung opacities measuring up to 3cm in diameter surrounded by lung parenchyma. There are a range of causes, benign and malignant. Benign causes include intrapulmonary lymph nodes, hamartomas, rheumatoid nodules and infective nodules (which will often disappear during surveillance) among others. Small nodules can, however, represent early malignancy such as lung cancer or metastatic disease and it is important that such nodules are managed appropriately.
Pulmonary nodules are generally incidental findings that are detected at imaging, most commonly CT, which is much more sensitive than chest radiography. Between 20 and 50% of CT scans find nodules, depending on the population and setting. Nodule detection is higher in CT screening for lung cancer. There are usually no symptoms caused by the nodule, even if the nodule represents an early lung cancer. It is important for the GP to know how to manage them, often in liaison with the secondary care ‘nodule’ service.
The management of a pulmonary nodule will vary depending on whether it has been detected on a chest x-ray or a CT scan. In this article, this will be considered as two separate problems.
CT is used far more commonly, with some GPs having direct access for patients with symptoms suggestive of lung cancer. Most rapid referral pathways for lung cancer now involve a CT prior to clinic appointment and the National Optimal Lung Cancer Pathway (NOLCP) recommends triage to appropriate clinics or discharge back to primary care.5 All this means that GPs may be faced with increasing numbers of incidental findings and the most common of these in this setting is pulmonary nodules. Furthermore, recent evidence has shown that screening for lung cancer in high risk individuals decreases mortality and screening of patients through ‘lung health checks’ is already underway in the UK, set in primary care, with encouraging initial results.1
CT scanning of the chest also takes place in secondary care with increasing frequency for a wide range of indications, such as investigation of suspected pulmonary embolism, trauma, and for suspected malignancy. GPs may encounter patients who have undergone CT scanning in these settings also, and ongoing management of nodules may be delegated to the patient’s primary care physician.
Current guidance is based on evidence from large screening trials such as NELSON, the Dutch-Belgian trial on CT screening for lung cancer.2 In the UK, the British Thoracic society (BTS) provides comprehensive evidence-based guidance on the management of small nodules detected incidentally on CT scans.3
Ignore
If a nodule is detected on chest x-ray, the GP should be guided by the radiologist’s report. Calcified nodules such as granulomas can be ignored, as can nodules that have clearly remained stable compared to previous imaging. The radiologist’s report will guide further management as to which nodules need to be imaged further with CT.
When nodules are detected incidentally at CT, nodule size is a strong determinant of further management. Nodules that measure 5mm or less in diameter, or more accurately, 80mm3 in volume (although not all centres perform volumetry), are not normally followed up (unless the patient is high-risk, for example, with a previous history of malignancy3, see figure 1). Larger nodules with clear evidence of benignity (such as fat in hamartomas or calcification in granulomas) can also be ignored. The radiologist’s report should provide guidance on whether referral is required.
Large screening trials2 have shown that participants with nodules below this size had no greater risk of malignancy than those with no nodules detected. The risk, however, although less than 0.5% is not negligible and patients should be advised of this.
Monitor/Refer
Patients who have nodules detected on chest radiographs highlighted in the radiologist’s report will generally need to be referred for a CT scan to characterise the nodule in more detail as well as provide information on staging. In this circumstance, the radiology report should provide advice on further management. Most pulmonary nodules detected by chest radiograph (not fulfilling ‘ignore’ criteria above) will be large enough to warrant referral to the respiratory service under the two-week wait rule, which will prompt a CT within three days as recommended by the NOLCP. Evidence suggests that delays in investigation and treatment of lung cancer are associated with adverse outcomes.4
Nodules detected by CT are often much smaller, and here a conservative approach is important. Patients with nodules over 5mm in diameter or 80mm3 in volume that are not clearly benign (either benign features or stable size/volume compared to previous imaging) will need to be referred to the respiratory service. Whether patients with nodules undergo surveillance or active management is determined by guidelines in consultation with the patient.3
A multidisciplinary team (MDT) meeting for pulmonary nodule management may be available for referral, this provides a platform for efficient management of patients with pulmonary nodules3 . Patients with small nodules (below 8mm) should be referred on a non-urgent basis for surveillance. A patient with a larger nodule that is of high risk for lung cancer may warrant referral directly to the lung MDT/respiratory service on a two-week wait. The radiology report should provide guidance on the level of suspicion in larger nodules and urgency of referral required – this may not be purely guided by size (although risk increases with size). Nodule features and growth compared to previous imaging and the presence of metastatic disease are important factors.
The pulmonary nodule MDT will normally triage referrals from a wide range of sources including GPs. The pulmonary nodule MDT coordinator will manage such referrals.
Patients with nodules detected during scans performed in secondary care should be referred by their physician but if the secondary care team is not respiratory, they may delegate this task to the primary care physician.
The BTS guideline3 outlines in detail management of pulmonary nodules incidentally detected at CT. Nodules measuring 5-8mm in diameter or between 80 and 300mm3 in volume are generally subject to surveillance, to detect interval growth (See figure 1). Interval CT scans are performed, usually at an initial interval of three months, followed by a year if there is no growth at this time. Semi-automated volumetry, if available to the reporting radiologist, is more accurate than measurement of nodule diameter for the detection of nodule growth and is therefore preferred. An example of volumetry in practice is illustrated in figure 1.
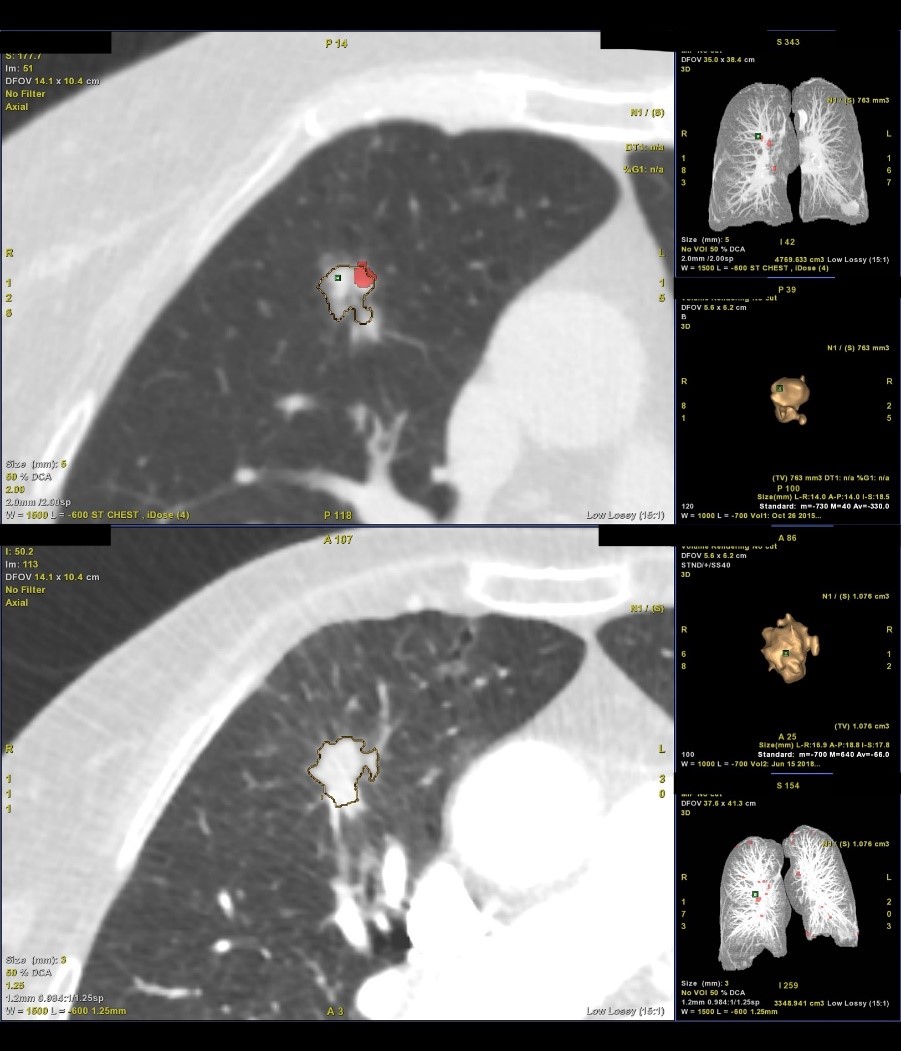
Figure 1: Demonstration of semi-automated volumetry and of a solitary pulmonary nodule (Lung VCAR, General Electric).
Top image – comparative volumetric analysis of a right upper lobe nodule, showing a clear increase in volume between the two scans. The larger images demonstrate outlining of the nodule by the software to calculate the volume. The smaller images in the right-hand column demonstrate the 3D reconstruction of the nodule and calculated volumes.
Middle and bottom image – the same pulmonary nodule demonstrating an increase in size over time, seen in the right middle lobe. The nodule has spiculated edges, which is a suspicious feature.
During surveillance, if the nodule increases in size, suggesting a neoplastic cause, the patient will be internally referred to the lung MDT for definitive management. This may involve consideration of a biopsy or surgery.
Brief overview of BTS guidance
The BTS guidance3 incorporates a series of algorithms for management of pulmonary nodules. Figure 2 demonstrates the initial management algorithm for pulmonary nodules detected incidentally at CT. The algorithm differs slightly in patients with sub-solid nodules (nodules that are either entirely, or partly, composed of ‘ground glass’) which are followed up for longer, but the principles remain the same. Patients are either discharged, undergo surveillance or are referred to the Lung MDT to undergo more active management.
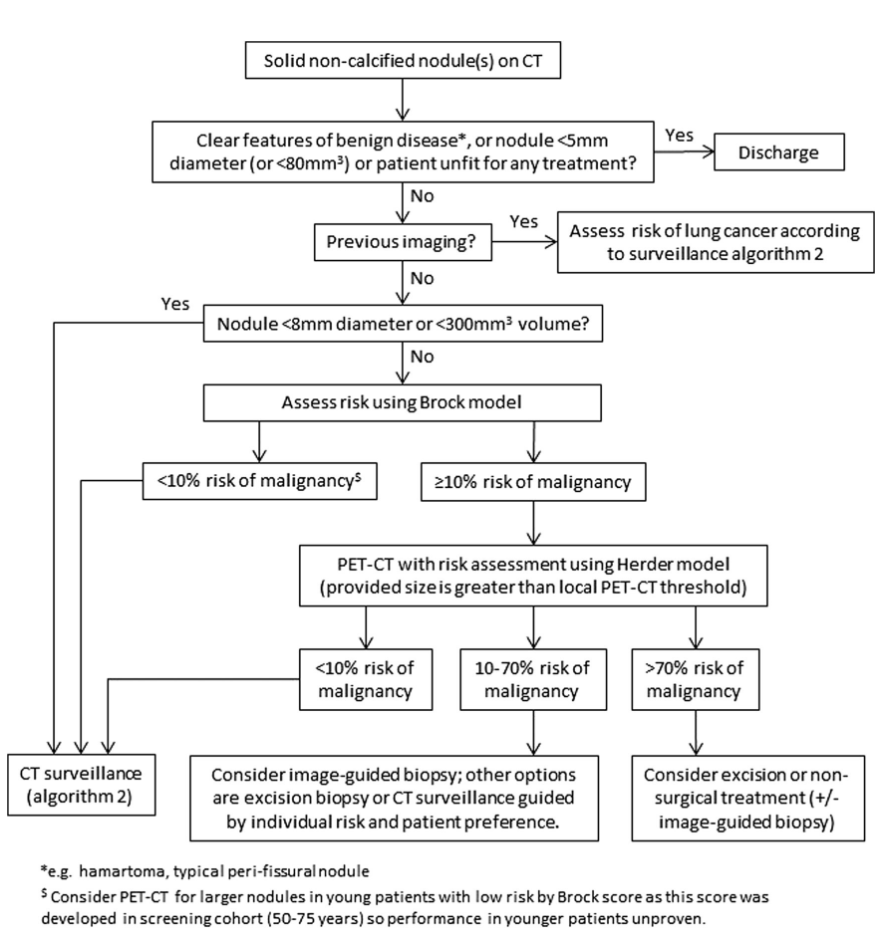
Figure 2: Initial approach to solid pulmonary nodule. Reproduced from with permission – see BTS Guidelines for pulmonary nodules 2015 for algorithm 2 and other management algorithms.3
In patients who are undergoing surveillance, scan intervals are fixed at three and 12 months. An interval of three months allows for detection of growth on volumetry but will also allow time for inflammatory nodules to resolve.
The guidance incorporates the use of multivariable risk prediction models to stratify patients by risk of lung cancer. This is used for larger higher risk nodules (see figure 2) that exceed 8mm in diameter. The Brock calculator is used to assess such nodules.6 Higher risk nodules (with a calculated risk of malignancy of over 10%) are usually further imaged with PET-CT. Further risk stratification thereafter is performed using the Herder model.7 The BTS has developed risk calculators to aid calculation of risk in a clinical setting.8 Patients who are deemed high risk (>10%) are generally referred to the lung MDT for further management.
Role of the GP in pulmonary nodule management
As well as organising initial referral to the appropriate service for management, the GP may have a key role during ongoing management and the pulmonary nodule service will update the referring GP (and the patient) by letter every time the patient is reviewed in the MDT. An understanding of the principles of management is therefore useful to the GP. Communication is very important, as nodule management is highly stressful for patients, who are worried about the possibility of cancer.9 Nodule management and implementation of screening programmes also provides an opportunity for GPs and other healthcare professionals to give patients advice on smoking cessation.10
Dr Iain Au-Yong is a consultant radiologist at Nottingham University Hospitals.
Professor David Baldwin is a consultant respiratory physician at Nottingham University Hospitals.
References
- Crosbie PA, Balata H, Evison M et al Second round results from the Manchester ‘Lung Health Check’ community-based targeted lung cancer screening pilot. Thorax. 2018 Nov 12. pii: thoraxjnl-2018-212547. doi: 10.1136/thoraxjnl-2018-212547.
- H De Koning, C Van Der Aalst, K Ten Haaf, M Oudkerk. Effects of volume CT lung cancer screening: Mortality results of the Nelson randomised controlled population based trial. International Association for the Study of Lung Cancer 19th World Conference on Lung Cancer (2018) Abstract: PL02.05
- Callister MEJ, Baldwin DR, Akram AR, et al. BTS Guidelines for pulmonary nodules. Thorax 2015;70: ii1–ii54.
- Diaconescu R, Lafond C, Whittom R. Treatment delays in non-small cell lung cancer and their prognostic implications. J Thorac Oncol. 2011 Jul;6(7):1254-9.
- https://www.cancerresearchuk.org/sites/default/files/national_optimal_lung_pathway_aug_2017.pdf
- McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013; 369: 910-919.
- Herder GJ, van Tinteren H, Golding RP, et al. Clinical prediction model to characterize pulmonary nodules: validation and added value of 18Ffluorodeoxyglucose positron emission tomography. Chest. 2005; 128:2490-2496.
- https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pulmonary-nodules/pn-risk-calculator/
- Slatore CG, Weiner RS. Pulmonary nodules: A small problem for many, severe stress for some and how to communicate about it. Chest (2018) Apr 153(4) 1004-1015
- https://www.brit-thoracic.org.uk/quality-improvement/guidelines/smoking-cessation/
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









