GP beware – genitourinary medicine

Case 1
The patient, a 45-year-old woman, attended her GP surgery with a complaint of vulval itch and soreness during intercourse. She had suffered with irritation and itching around the vulva for the last six weeks. She reported no notable vaginal discharge. Of note, she had attended surgery on four other occasions in the preceding two years with vulval itch, and was treated presumptively for thrush on each occasion, receiving general advice on vulval hygiene and the use of emollients, with partial resolution of her symptoms each time. Given the chronicity of her symptoms, the GP examined her and found marked sclerotic changes to the vulval skin. The patient was advised to attend the local GU clinic for further management.
GP’s diagnosis
Candidiasis.
Actual diagnosis
Lichen sclerosus.
Clues
Symptoms of vulval itch in an older woman with no other clinical signs to suggest a candidal infection should be investigated for other causes of vulval itch, including dermatitis, eczema and lichen sclerosus. Clinical examination in the GU clinic demonstrated features of lichen sclerosus – thickened, whitened skin with surface telangiectasiae affecting the vulva and extending to the perineum and anus, with involutional changes of the labia minora and clitoris.
Take-home message
Lichen sclerosus is a poorly understood dermatosis of possible autoimmune-mediated inflammation, mainly affecting the vulval and anogenital areas in women, and the glans penis and foreskin in men. If left untreated, the disease is progressive and can cause permanent architectural changes and secondary sexual dysfunction. It often presents insidiously with itching and sometimes dyspareunia in women, and with lower urinary tract symptoms or foreskin problems in men. If untreated, the disease is associated with a progression to squamous cell carcinoma in some cases. It has typical clinical features on examination, and repeat attendances such as this should have prompted a genital examination. She was referred to a dedicated vulval dermatology service. Lichen sclerosus can be effectively managed with hyperpotent topical steroids, and patient self-management.
Case 2
A young, Caucasian, otherwise fit and healthy man attends your surgery with symptoms of occasionally bloody diarrhoea, associated with mucoid discharge and a sense of incomplete emptying. This has been the case for two weeks. Tests are sent for inflammatory markers, a coeliac screen, and a faecal calprotectin.
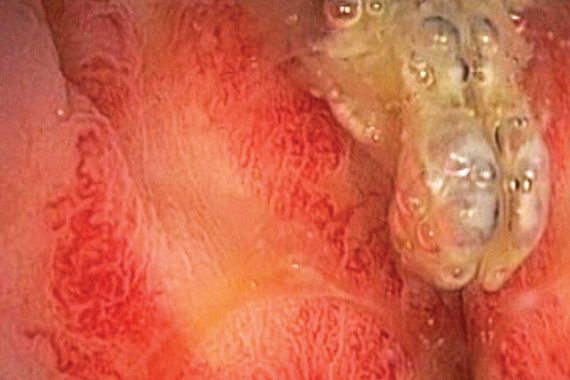
All tests come back elevated and he is referred urgently to gastroenterology for a workup for inflammatory bowel disease (IBD). He is sent for a colonoscopy, which shows inflammation with ulcer formation to the recto-sigmoid junction, and he is started on steroid therapy to treat active IBD. Histopathology confirms an abscess formation, patchy active colitis and inflammatory granulation tissue.
The patient fails to respond to steroids. He volunteered that he was a gay man, having had multiple casual sexual contacts with receptive anal sex in the preceding few months, and asked if he might have an STI. A swab was taken from the rectum for Chlamydia trachomatis testing. This was positive, with evidence of lymphogranuloma venereum-specific (LGV) DNA.
GP and gastroenterologist diagnosis
IBD.
Actual diagnosis
Infectious proctitis caused by LGV.
Clues
LGV is an STI caused by one of three invasive serovars (L1, L2 or L3) of Chlamydia trachomatis. LGV used to be rare in industrialised countries since the mid-1960s. Since 2003, however, there have been a series of LGV outbreaks reported across Europe, occurring mostly among HIV-positive men who have sex with men (MSM). LGV is now considered to be hyperendemic in the UK, with 400 to 500 cases reported annually for the last few years. It typically presents with a proctocolitic syndrome developing over weeks, sometimes with systemic features. It may mimic the signs of IBD.
Endoscopies can look macroscopically similar with proctitis, inflammation and granuloma formation, and histology may be indistinguishable. However, LGV is readily treated with a three-week course of doxycycline 100mg bd. This patient was referred to the GU clinic for further management and screening for other infections. Owing to the duration of his untreated infection, he had developed a rectal stricture, which persisted despite clearance of the underlying infectious process.
Take-home message
This case emphasises the value of taking a sexual history in people presenting with genitourinary symptoms, which includes the anus and rectum in anoreceptive MSM. Studies suggest a substantial proportion of MSM are not ‘out’ to their GP. Had a sexual history been taken sooner, referral to the GU service or an earlier consideration of an STI pathogen may have prevented irreversible complications.
Case 3
A 45-year-old gentleman presents to his GP with symptoms of dysuria, strangury, nocturia and incomplete emptying, in association with dull lower back pain and penile tip pain. He has attended for the same issue on two occasions over the preceding six months, and he tends to improve after a short course of antibiotics, but relapses shortly after. Serial mid-stream urine samples are sterile, but white cells are present. A serum PSA is 2.28mg/l. An ultrasound of the renal tract is normal, with normal bladder emptying. He is advised to attend the GU clinic to rule out an STI.
GP’s diagnosis
Recurrent UTI.
Actual diagnosis
Chronic bacterial prostatitis.
Clues
The spectrum and chronicity of symptoms is suggestive of prostatitis. Further questions revealed a history of mild erectile dysfunction, pain on ejaculation, and post-ejaculatory burning. A semen culture was positive for Escherichia coli. An MRI scan showed a structurally normal prostate, but with peripheral enhancement post-contrast, supporting the diagnosis. The patient received prolonged antimicrobial therapy, as directed by the sensitivity of the underlying organism, and a short course of α-blockers. He was much improved at three-month follow-up.
Take-home message
Recurrent UTIs in men should be questioned, and prostatitis should be considered in all age groups. Prostatitis is common, but symptoms are non-specific and variable, and it is often misdiagnosed. Treatment requires prolonged antimicrobial therapy, and a holistic approach. A proportion of men will develop chronic pelvic pain or lower urinary tract symptoms if left untreated.
Dr Michael Rayment is a consultant in HIV and sexual health at Chelsea and Westminster NHS Foundation Trust
Dr Sharanjit Dhoot is a specialty doctor in genitourinary medicine and HIV at Chelsea and Westminster NHS Foundation Trust
Dr Taslima Rashid is a specialty registrar in genitourinary medicine and HIV at Chelsea and Westminster NHS Foundation Trust
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









