What to do with incidental ovarian cysts
Presentation
An incidental finding of an ovarian cyst suggests that a patient has presented with little to no symptoms. Typically, ultrasound scans are requested in females for menstrual irregularities such as intermenstrual bleeding, postcoital bleeding, heavy menstrual bleeding or postmenopausal bleeding, or for pelvic pain or prolapse symptoms. Pelvic pain may encompass cyclical pain, usually during or just before menstruation, or pain outside the menstrual cycle. Mid-cycle pain may reflect ovulation.
The pain of a symptomatic ovarian cyst (>50mm) is typically sharp, stabbing and intermittent. A pain that is constant and severe, and may subsequently stop suddenly, should raise concerns about ovarian torsion or cyst accident. An acute cyst accident may also present with vomiting.
It is important to rule out other causes of these symptoms, such as endometriosis, which presents with cyclical pain, and inflammatory bowel disease, which can present with bloating, pelvic or abdominal pain and altered bowel habit. Uncommonly, a large ovarian cyst can present as a prolapse through the vagina. A careful history of symptoms, relevant gynaecological history and family history should be taken.
Ignore
A transvaginal ultrasound scan is preferable to a transabdominal ultrasound for diagnosis as it has increased sensitivity. The IOTA (International Ovarian Tumour Analysis) group has devised a ‘simple rules’ ultrasound classification system that predicts a benign tumour (B-rules) based on a set of ultrasound features. It is used by experienced radiologists to calculate risks if there are uncertain features on ultrasound. Commonly, a conclusion about risk is given in the final ultrasound report.
These features include:
- Unilocular cyst.
- Largest solid component smaller than 7mm in diameter.
- Presence of acoustic shadowing.
- Smooth, multilocular mass smaller than 100mm.
- No blood flow on Doppler.
The presence of one or more of these features suggests the woman can be reassured that the cyst is benign.
A simple cyst (as defined by the IOTA above criteria) smaller than 50mm, particularly in a woman with minimal symptoms, will usually resolve spontaneously over the next three menstrual cycles and therefore does not require follow-up. For postmenopausal women, see below.
Monitor
Women with a simple ovarian cyst of 50-70mm should have yearly ultrasound follow-up, as enlarging cysts may cause pain and ovarian accidents such as torsion or cyst rupture. Women with cysts larger than 70mm, particularly with symptoms, should be referred to a gynaecologist for discussion regarding further assessment and removal.
In postmenopausal women with a simple cyst smaller than 50mm, follow-up ultrasound should be every four to six months, with repeat CA125 levels. If after one year of follow-up the cyst remains stable or reduces in size, and the CA125 is within normal limits, it is reasonable to discharge the woman from follow-up.
Measurement of serum CA125 is not usually required in premenopausal women with ultrasound features of a simple ovarian cyst. CA125 is an unreliable marker for the detection of ovarian cancer as only 3% of the presenting population with a raised CA125 will have ovarian cancer, and only around 50% of women with early ovarian cancer will have a raised CA125. This serum marker is also raised in multiple benign conditions such as endometriosis, fibroids and pelvic infection, as well as liver cirrhosis, diverticulitis, inflammatory bowel disease and even pregnancy. Serum CA125 is produced from the epithelium of the ovary but can also be produced in response to irritation or inflammation of the peritoneum. A more sensitive marker, serum HE4, has been suggested as a marker for ovarian cancer as it is less frequently elevated in benign tumours or endometriosis.
A complex cyst is defined as a multilocular cyst containing solid components. If a complex ovarian mass is detected on an ultrasound scan, a CA125 level should be measured and referral made to secondary care. An initial CA125 level greater than 200IU/ml (normal is <35IU/ml) should raise suspicion of malignancy and prompt urgent referral (see below). Women with a normal CA125 or a value greater than 35IU/ml (but less than 200IU/ml) with normal ultrasound scan findings, should be assessed for other causes. Those with persistently raised CA125 levels with no other identified cause should be referred to secondary care.
In a woman under the age of 40 with a complex ovarian mass who has been referred to secondary care, serum HCG, AFP and LDH will be performed in addition to CA125, as these women carry a greater probability of a non-epithelial ovarian cancer, such as a germ-cell tumour.
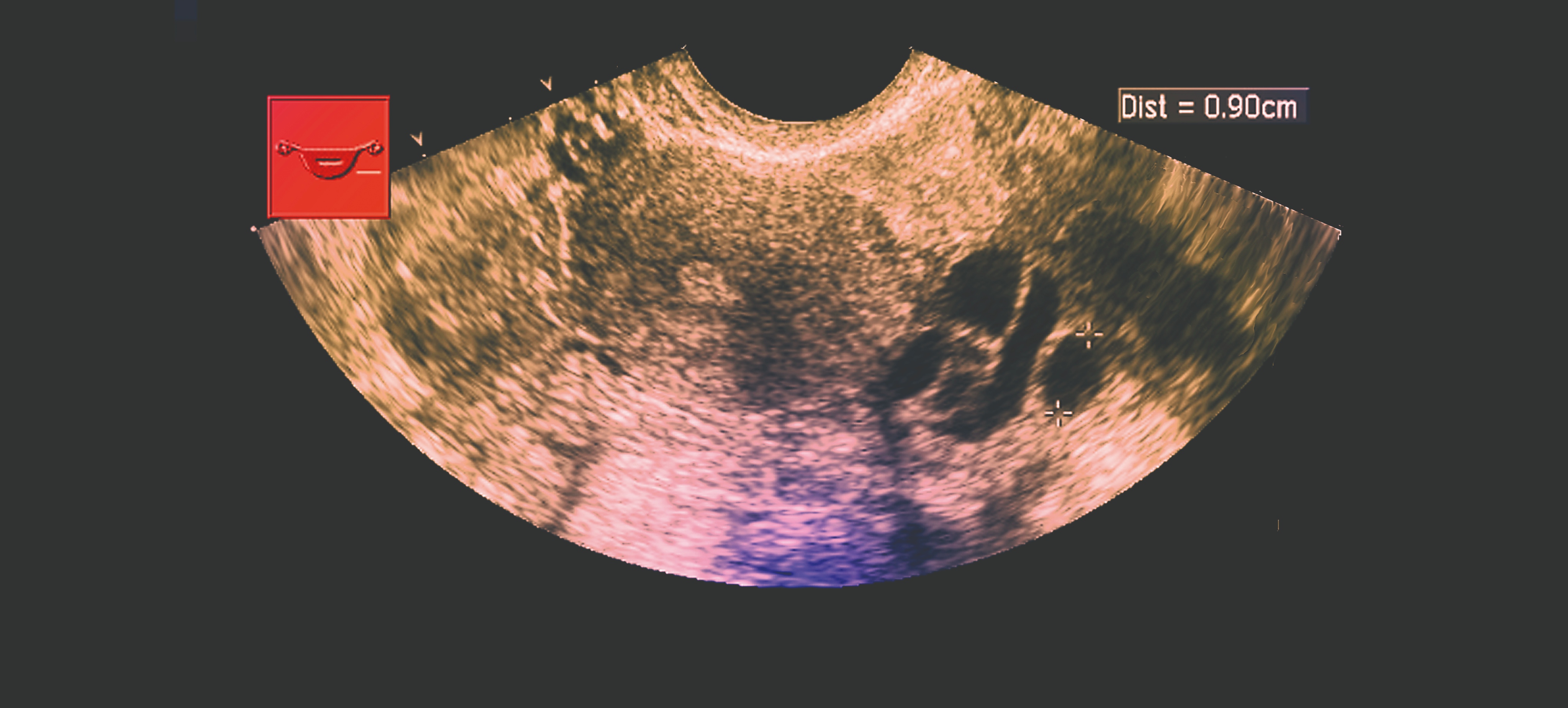
Transvaginal ultrasound showing ovarian cysts
Refer
Ovarian cysts that persist over several cycles in premenopausal women, particularly if they are symptomatic, or those that increase in size, should be referred to secondary care. These cysts may need to be removed surgically (typically by laparoscopy), and therefore referral to a general gynaecologist should be made even if there are no features of a malignancy.
Although the majority of cysts are benign, it is important to recognise those that may be malignant. Occasionally there may be incidental ultrasound findings of a malignant pelvic mass with ascites.
The IOTA group ultrasound features of suspected malignant ovarian mass (M-rules) are:
- Irregular solid tumour.
- Presence of ascites.
- Four or more papillary structures.
- Multilocular solid tumour with largest diameter of 100mm or more.
- Strong ultrasound Doppler blood flow.
Any of the features above should prompt urgent referral to a gynaecological oncologist. A CT scan with or without MRI of the pelvis may then be requested for further assessment.
Using the CA125 result and certain ultrasound features, a risk of malignancy (RMI) score can be calculated and used as an alternative to the IOTA rules, for those women with suspected ovarian malignancy (see table, left). An RMI of more than 250 should prompt referral to a gynaecological oncology centre for multidisciplinary team discussion on a two week-wait basis. Other risk-scoring algorithms have been described, including risk of ovarian malignancy algorithm (ROMA), which uses a woman’s CA125, HE4 and menopausal status to estimate the probability of ovarian cancer.
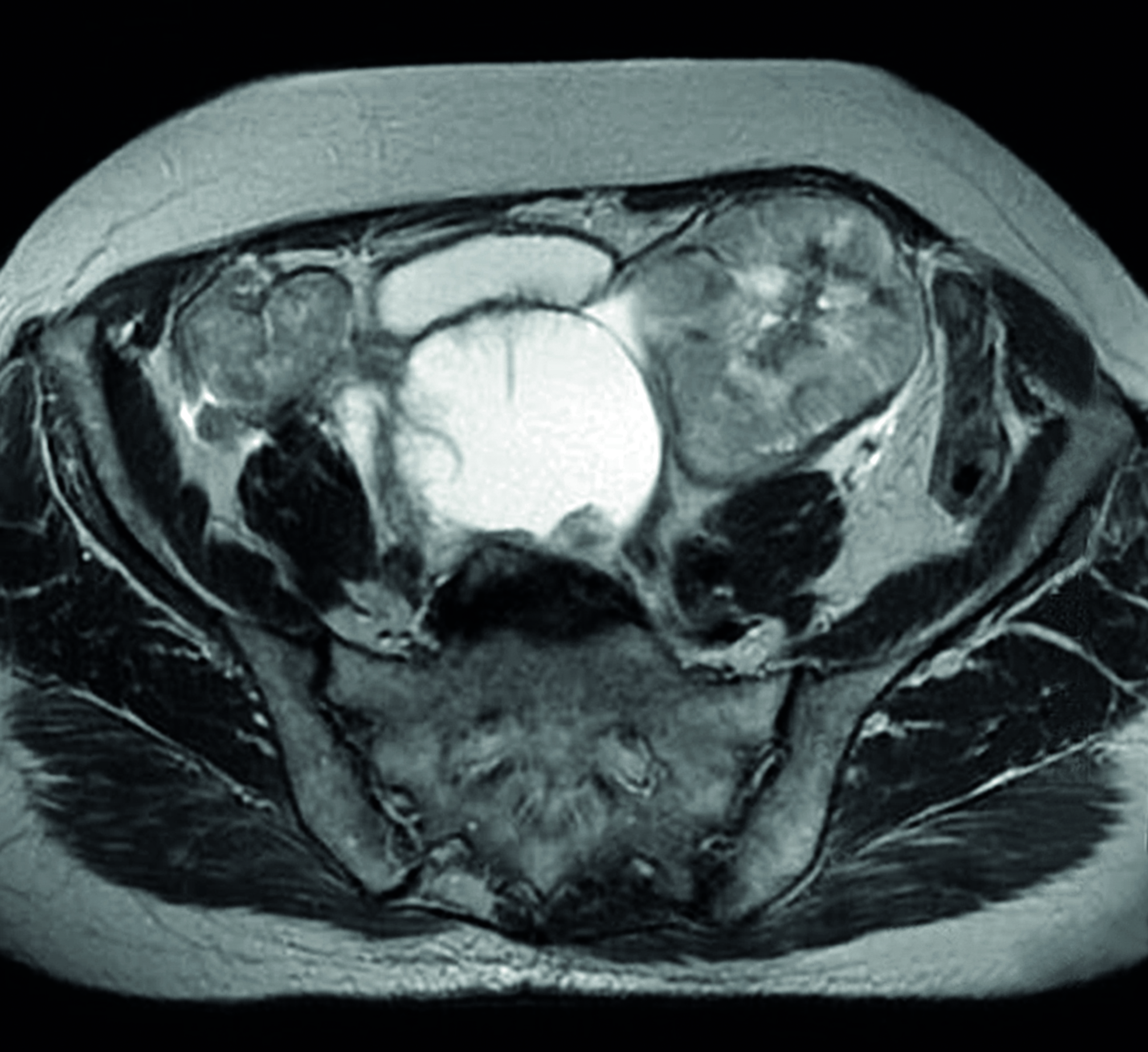
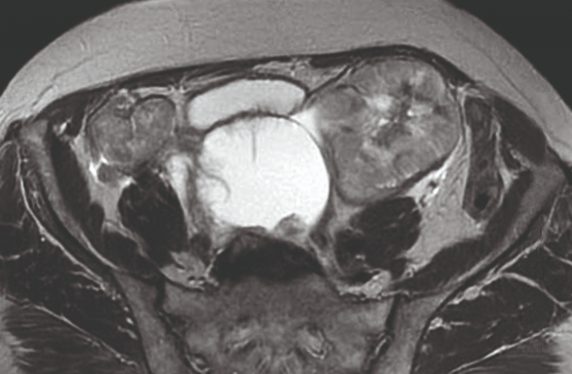
MRI scan showing bilateral ovarian cancer
RMI algorithm
RMI score = U x M x CA125 (4)
- U: ultrasound score
- One point scored for the presence of each of the following features: multilocular cysts; solid areas; metastases; ascites; and bilateral lesions. U=0 (0 points), U=1 (1 point) or U= 3 (2-5 points).
- M: menopause score
- M=1 (premenopausal) or M=3 (postmenopausal). The classification of ‘postmenopausal’ is a woman who has had no period for more than one year or a woman over 50 who has had a hysterectomy.
- CA125 Serum CA125 concentration – measured in IU/ml
Dr Stacey Bryan is a research fellow in gynaecological oncology and Miss Adeola Olaitan is a consultant gynaecological oncologist, at University College Hospital, London
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.










