Women’s health: Menopause and HRT


GP Dr Nazia Hussain discusses HRT for the non-specialist as part of our Pulse Live series, showcasing the best sessions from our flagship live events
With increased patient awareness of menopause and hormone replacement therapy (HRT), it is important that primary care teams feel confident discussing issues such as diagnosis, symptoms, investigations, HRT types, HRT risks versus benefits, appropriate review and when to refer.
Background
These are the definitions of menopausal stages:1
- Menopause is diagnosed clinically after 12 months of amenorrhoea. In the UK, the average age of natural menopause is 51 years.
- Perimenopause is the period before the menopause, characterised by irregular cycles.
- Post menopause is the time after there has been no menstrual period for 12 months.
- Early menopause is cessation of ovarian function between 40-45 years.
- Premature menopause is loss of ovarian function before 40 years.
With increased life expectancy, women are postmenopausal for more than a third of their lives, on average. Around 75% experience symptoms; around 25% experience severe symptoms, which negatively impact their lives.
Vasomotor symptoms are the most well-known, but symptoms include: low mood, anxiety, reduced self-esteem, poor memory and concentration, reduced libido, joint pains, vaginal dryness, bladder issues, and worsening migraine2.
Diagnosis
Follicle-stimulating hormone (FSH) testing is not required to confirm the diagnosis of menopause in those aged > 45 if (a) they have vasomotor symptoms and irregular periods (b) the last menstrual period (LMP) was > 12 months ago and they are not using hormonal contraception or (c) they have symptoms of menopause and no uterus3.
Consider testing in those aged 40-45 with menopausal symptoms, including a change in their menstrual cycle, and those aged < 40 in whom menopause is suspected3.
Hormones can affect testing. Testing is NOT valid in women taking combined oestrogen/progesterone contraception/HRT. The progesterone-only injection can suppress FSH. The optimum time to measure is just before the next injection. If a woman is using the injection and the FSH is raised, the increased levels are due to perimenopause4.
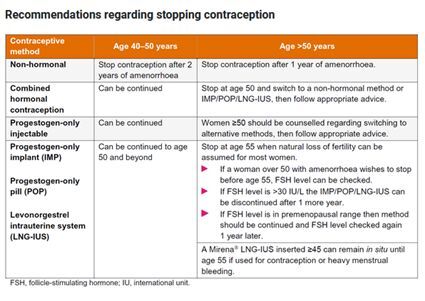
When to stop contraception
The Faculty of Sexual and Reproductive Healthcare (FSRH) has produced a very useful table outlining advice about when it is appropriate to stop contraception5.
Managing symptoms
Vasomotor symptoms
Offer HRT, discussing risk and benefits6. Do not routinely offer alternatives to HRT eg, gabapentin, pregabalin, clonidine, SSRIs (eg, fluoxetine, citalopram), SNRI (eg, venlafaxine) first-line, but these are options if needed7.
Herbal preparations such as isoflavones, St John’s Wort or black cohosh may relieve symptoms, but safety issues, variability of preparations available and potential drug interactions indicate they should only be used with caution.
Psychological symptoms
Use HRT or refer for cognitive behavioural therapy. There is no evidence for using anti-depressants to treat low mood in menopausal women not diagnosed with depression.
Altered sexual function
Consider referral for testosterone supplementation for menopausal women with low sexual desire if HRT alone is not effective8.
Urogenital atrophy
Offer vaginal oestrogen. This can be used together with systemic HRT eg, creams (Gynest, Ovestin), vaginal tablets (Vagifem 10, Vagirux 10), vaginal ring (Estring 3 monthly), vaginal pessary (Imvaggis), vaginal gel (Blissel). Continue treatment for as long as needed to relieve symptoms. Seek advice from a menopause specialist if systemic HRT is contraindicated before using. Patients should report unscheduled vaginal bleeding, but there is no need to monitor endometrial thickness. Vaginal oestrogen can be used with moisturisers and lubricants eg, Yes, Sylk, Regelle, Hyalofemme, Replens MD9.
Which HRT and when?
- Oestrogen forms part of all HRT and the safest route is transdermal.
- Decide if progesterone is needed. It should be given if the uterus or any endometrial tissue is present to avoid endometrial hyperplasia e.g. subtotal hysterectomy, endometriosis.
- Decide if HRT should be sequential or continuous ie, is the progesterone component going to be given intermittently cycling or continuously. Consider whether if there is unstable endometrium that will cause irregular bleeding if continuous HRT is used too early.
Oestrogen
The risk of VTE associated with HRT is greater for oral than transdermal preparations. Consider transdermal rather than oral HRT for menopausal women who are at increased risk of VTE, including those with a BMI over 30 kg/m2. Transdermal oestrogen can be prescribed via gels (eg, Oestrogel 2-4 pumps a day, Sandrena gel 0.5mg/1mg sachets), patches (eg, Evorel 25 / 50 / 75 / 100 mcg patches twice a week; Estradot 25 / 50 / 75 / 100 mcg patches twice a week; Elleste 40 / 80mcg patches twice a week) or topical spray (Lenzetto 1-3 sprays daily).
If a patient prefers to use oral oestrogen, the safest in terms of clot and breast cancer risk contain dydrogesterone:6 the Femoston range.
Sequential Options Continuous Options Femoston 1/10 (1mg estradiol/ 10mg dydrogesterone) Femoston Conti 0.5/2.5 (0.5mg estradiol/ 2.5mg dydrogesterone) Femoston 2/10 (2mg estradiol/ 10mg dydrogesterone) Femoston Conti 1/5 (1mg estradiol/ 5mg dydrogesterone)
The British Menopause Society provides a useful document to advise on HRT and equivalent preparations, especially in times of supply shortage10.
Progesterone
Progesterone should be given as part of HRT if the uterus or any endometrial tissue is present to avoid endometrial hyperplasia. This can be delivered:
- as part of a combined patch preparation (e.g. Evorel Sequi for perimenopause/ Evorel Conti for post-menopause)
- as separate progesterone tablets. Utrogestan is available as 100mg capsule each evening as continuous HRT for post-menopause (licensed for days 1-25 but easier to take every night); 2 x 100mg capsules each evening for 2 out of 4 weeks as sequential HRT for perimenopause (licensed for days 15-26 but easier to take for 2 weeks; sometimes given vaginally off-licence)11.
- as a 52mcg levonorgestrel-containing intra-uterine device. This would be ideal to offer both contraception and endometrial protection. The FSRH states that only the 52mcg containing coils should be used for endometrial protection and they can be used for 5 years (which may be different from the licence) 5. The 3 brands containing 52mcg are Mirena, Benilexa and Levosert.
Sequential or Combined HRT?12
Sequential HRT is used if ‘unstable endometrium’ is present to give better bleeding predictability. This is likely when the LMP is < 12 months ago or there is regular bleeding ongoing.
Continuous HRT is used if ‘stable endometrium’ is present. It is safer and less likely to cause endometrial proliferation. If used in a patient with unstable endometrium, it is more likely to produce irregular bleeding patterns and may result in unnecessary investigations. Stable endometrium is more like in a patient when the LMP is > 12 months ago, the patient is amenorrhoeic from contraception eg, progesterone only injection/ implant/ pill, they are aged > 54.
Review and referral12
Review after three months then annually. Remember breast and cervical screening reminders. If HRT is not helping, consider dose increase or change in formulation or delivery route.
Refer if there has been no improvement in symptoms or the patient has ongoing troublesome side-effects.
Referral may also be appropriate if the patient has contraindications or cautions to HRT eg, venous thrombo-embolism, undiagnosed vaginal bleeding or untreated endometrial hyperplasia, oestrogen-sensitive cancer, breast cancer, porphyria cutanea tarda, active liver disease with abnormal liver function, active/recent arterial thromboembolic disease, or bleeding issues
Unscheduled bleeding is common up to six months after starting HRT. Consider pregnancy risk, STI risk and cervical cytology history/ examination. Investigate (via pelvic ultrasound +/- referral for hysteroscopy:
- new change in bleeding pattern eg, new inter-menstrual bleeding, post-coital bleeding
- new bleeding after a time of amenorrhoea
- if there is continued bleeding after using continuous HRT for six months
HRT Risks vs. Benefits11
For most women, the benefits of HRT outweigh the risks when initiated within 10 years of menopause. Benefits include control of menopausal symptoms and maintenance and improvement of bone mineral density. HRT also reduces the risk of osteoporotic fractures, coronary heart disease, Alzheimer’s disease, colorectal cancer and type 2 diabetes.
Endometrial cancer
Risk increases if oestrogen-only HRT is given when the uterus/ endometrial deposits are present. This is reduced by adding progestogen. Continuous progesterone provides better long-term protection vs. cyclical.
Venous thromboembolism
Risk increases with oral HRT (relative risk = 2), but there is no increased risk with transdermal HRT. Consider using transdermal HRT first-line, especially in those with risk factors e.g. BMI > 30.
Heart Disease
Risk increases when oral HRT is started at over age 60 or in those with pre-existing disease. The first 10 years after menopause is a cardiovascular ‘window of opportunity’. The presence of risk factors is not a contraindication, as long as they are optimally managed. HRT with oestrogen alone is associated with no or reduced risk. HRT with oestrogen and progestogen is associated with little or no increased risk.
Stroke
Risk increases when oral HRT is started at over age 60. There is no increased risk with transdermal oestrogen.
Breast cancer
Risk increases slightly after a minimum of five years’ use combined HRT. The risk with oestrogen alone is very much less. Mortality is not increased. The risk is lower with micronised progesterone compared with synthetic. The risk is related to treatment duration and reduces after stopping HRT.
Migraine and HRT13
Fluctuating oestrogen with vasomotor symptoms in menopause can increase the frequency of migraine. Migraine with aura does not contraindicate HRT, but avoid oral oestrogen. Use the lowest effective dose of transdermal oestrogen. Where progestogen is required, continuous delivery is recommended eg, a levonorgestrel-containing coil. Consider non-HRT options for vasomotor symptoms eg, venlafaxine.
Quality Improvement activity
Audit ideas:
- Are all patients prescribed oestrogen-only HRT coded as having had a hysterectomy?
- Did the last 20 patients who had FSH testing really need it?
- What proportion of patients are prescribed oral vs. transdermal HRT? Consider a medication review to switch to safer transdermal routes where appropriate.
Dr Nazia Hussain is a GP in Wales with a special interest in women’s health and migraine

Pulse 365 LIVE Events cover a broad array of topics pertinent to you, your patients, and your practice. You will gain free CPD and be able to take part in live Q&As. Specifically created for all practising, GMC-registered GPs and trainees, you will hear from experts across primary and secondary care, and network with like-minded GPs. Sign up for your nearest event today.
References
- NICE Clinical Knowledge Summaries: Menopause. Last reviewed September 2022. https://cks.nice.org.uk/topics/menopause/
- HRT Easy Prescribing Guide. Newson Health Menopause Society. https://www.nhmenopausesociety.org/resources/easy-hrt-prescribing-guide/.
- Menopause: diagnosis and management. NICE guideline [NG23] November 2015 Last updated: 05 December 2019. https://www.nice.org.uk/guidance/ng23
- GP Notebook. FSH Measurement if on Contraception. https://gpnotebook.com/en-gb/simplepage.cfm?ID=x20130226163512685340&linkID=75831
- FSRH Clinical Guideline: Contraception for Women Aged over 40 Years (August 2017, amended September 2019). https://www.fsrh.org/documents/fsrh-guidance-contraception-for-women-aged-over-40-years-2017/
- Guidance on management and prescribing HRT for GPs. Dr Imogen Shaw. https://pcwhf.co.uk/resources/guidance-on-management-and-prescribing-hrt-for-gps/
- British Menopause Society. Prescribable alternatives to HRT. https://thebms.org.uk/wp-content/uploads/2022/12/02-BMS-TfC-Prescribable-alternatives-to-HRT-NOV2022-A.pdf
- British Menopause Society. Testosterone replacement in menopause. https://thebms.org.uk/2019/02/testosterone-replacement-in-menopause/
- Menopause Matters. Vaginal problems: treatments https://www.menopausematters.co.uk/dryness.php
- British Menopause Society. HRT preparations and equivalent alternatives. https://thebms.org.uk/2022/01/hrt-preparations-and-equivalent-alternatives/
- GP Notebook. Brief Practical Guide to HRT. https://gpnotebook.com/en-gb/simplepage.cfm?ID=x20200220132547335581
- North Yorkshire and York Menopause Guidance – HRT. https://northyorkshireccg.nhs.uk/wp-content/uploads/2021/11/Primary-care-HRT-guidelines-v15.pdf
- British Menopause Society. HRT and Migraine. https://thebms.org.uk/2017/11/migraine-and-hrt/
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.
Related Articles
READERS' COMMENTS [1]
Please note, only GPs are permitted to add comments to articles











To cause one extra case of breast cancer, treat 100 women with combination hrt for ten years; is that a “small” risk?
Multiply that by thousands of women?