GP trainers among those at highest risk of burnout, GMC warns
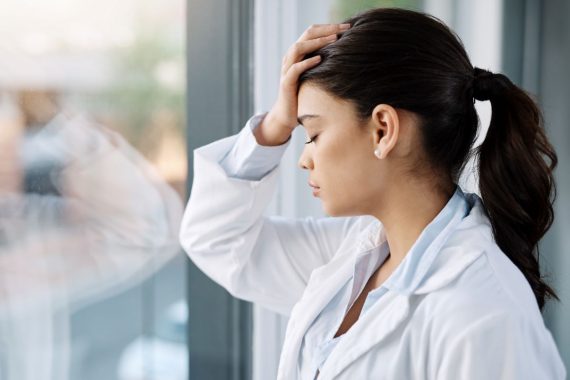
GP trainers are more at risk of burnout than the average for all specialties, according to the GMC’s annual training survey results.
The survey of over 70,000 doctors who are trainees or trainers found that 15% of GP trainers are at high risk of burnout, which is higher than the average of 12% and ranked second only to emergency medicine at 24%.
The results also showed that 24% of GP trainers said that every working hour is tiring for them, compared to 11% of public health trainers.
Last month, GP leaders raised concerns about how trainers and experienced GPs will handle the long-term workforce plan’s expansion of training places, especially given the existing pressures and lack of retention measures.
The plan pledged a doubling of medical school places to 15,000 and an increase in GP training places by 50% to 6,000 by 2031.
Similar pressures were evident for GP trainees in the survey results, with just over one fifth (21%) at high risk of burnout, which is up from 18% last year and ranked roughly in the middle among other specialties.
For the first time, the GMC included questions on experiences of discrimination, and the results showed that more than a quarter (27%) of trainees said they experience microaggressions, negative comments, or oppressive body language from colleagues.
In March, a report by the GMC laid bare the inequalities experienced by medical trainees from different ethnic backgrounds
However, GP trainees were among the specialties with the lowest rates, with 13% of this cohort reporting these experiences, compared with 35% of trainees in emergency medicine.
The report also found that GP trainees and trainers were ‘more positive about the supportive nature of their working environment than those working in secondary care’.
According to the results, 94% of GP trainees and 98% of GP trainers said their practice provides a supportive environment for everyone, regardless of background, beliefs, or identity, compared to 87% of trainees and 78% of trainers in secondary care.
But GP trainees seemed to be doing more overtime, with 16% saying they worked beyond their rostered hours on a daily basis, compared to only 1% of anaesthetics trainees saying this was the case.
The GMC’s medical director and director of education and standards Professor Colin Melville said some of the survey’s findings are ‘worrying’, and that discrimination affects not just individuals but ‘teamwork, communication and potentially patient safety’.
He also said: ‘We are seeing continuing proof of pressures affecting trainers, including increasing rates of burnout and difficulties with finding adequate time to provide training.
‘The recent publication of NHS England’s long term workforce plan was welcome, but efforts to expand medical education will falter without a focus on the number, needs and wellbeing of trainers.’
Responding to the GMC’s survey results, deputy chief executive at NHS Providers Saffron Cordery said they are ‘concerned many trainers feel burnt out to the point where they feel they don’t have the time to deliver training’.
She said: ‘This inevitably impacts morale, which in turn impacts retention. The new long-term workforce plan promises to tackle staff burnout through measures including increasing the workforce. But for trainers to be able to educate new staff, their wellbeing must also be protected.’
Chair of the RCGP Professor Kamila Hawthorne said the college has long warned of the need to ‘address excessive workforce and workload pressures’ to stop trainees leaving the profession ‘before or shortly after they qualify’.
She said: ‘We want to create a supportive environment for our trainees, so they can deliver safe, timely and effective patient care, while developing the skills they need to fully-qualify for independent practice.
‘However, they are doing so in the context of demand that is growing both in volume and complexity – with both trainees and qualified GPs stretched beyond healthy limits.’
The BMA council’s deputy chair Dr Emma Runswick said the survey results further show ‘the severe toll that the pressures of understaffing and lack of support is having on doctors’ wellbeing’.
She said: ‘This survey also highlights how – alongside known impacts on workload, wellbeing and waiting times – vacancies and rota gaps are negatively affecting doctor training. Without enough staff, the quality of training suffers, and therefore we cannot create a better NHS for the future.
‘Doctors and their colleagues are treading water to keep their heads above the surface and this is not sustainable for them, the health service or patients.’
In April, NHS England introduced a new QOF indicator which focussed on reducing the risk of GP and practice staff burnout.
The GMC’s survey had responses from 49,022 trainees and 21,689 trainers.
Specialty variation for trainers at high risk of burnout (2023)
All trainers – 12%
- Emergency medicine – 24%
- General practice – 15%
- Obstetrics and gynaecology – 15%
- Paediatrics and child health – 13%
- Ophthalmology – 11%
- Surgery – 11%
- Psychiatry – 11%
- Medicine – 11%
- Pathology – 11%
- Public health – 10%
- Radiology – 10%
- Anaesthetics – 9%
Related Articles
READERS' COMMENTS [4]
Please note, only GPs are permitted to add comments to articles










Well, this is great news for the GMC. It gives them another group of doctors to closely look at, as the witch-hunter general, and given the information, Trainers will be even more “guilty until proved innocent”.
GMC- lower than vermin.
I’ll say it again——-you do not need to train to be a G.P.———I never did
Dealing with the RCGP and their minions does tend to be a little frustrating. Quite what they are training trainees for is increasingly mysterious.
Trainees have an extensive of knowledge of which inhalers to use to save the planet, and extensive knowledge of equality, diversity and something known as variance; but they cannot identify even common rashes, and consequently we are now dealing with an expanding outbreak of imaginary scabies in the local student population.
scabies isn’t always an easy diagnosis to be fair – we have all dished out a bit of unnecessary derbac in our time
but i can see how mass hysteria could soon develop in an excitable demographic