Women at high risk of breast cancer told to see GP to access preventive drug
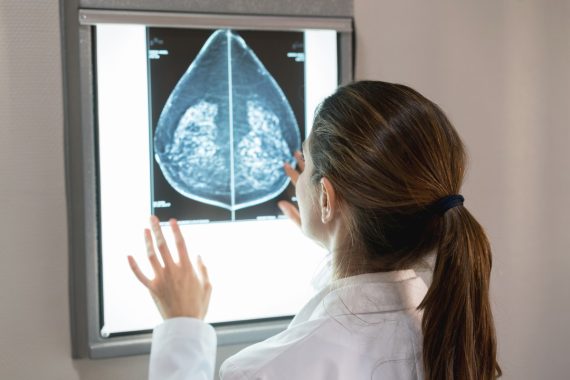
NHS England has encouraged thousands of women at high risk of breast cancer to see their GP about a repurposed drug to prevent breast cancer.
The Medicines and Healthcare products Regulatory Agency (MHRA) has today licensed anastrozole for use to help prevent the disease, and trials have shown that it can reduce incidence by almost half.
The drug, which is currently used as a breast cancer treatment, is ‘more attractive’ than its predecessor tamoxifen, according to NHS England’s national clinical director for cancer Professor Peter Johnson.
Speaking to BBC Radio 4 this morning, Professor Johnson said that for women with a ‘strong family history’ of breast cancer, the suitability of anastrozole is ‘something to discuss with your GP’.
There are almost 300,000 post-menopausal women at moderate or high risk of the disease who could be eligible for the drug, and GPs have highlighted concerns around their capacity to deal with this potential influx of patients.
Chair of the BMA’s GP Committee in England Dr Katie Bramall-Stainer said the licencing of anastrozole is ‘fantastic news’ but criticised NHS England’s lack of consultation with GPs.
In a post on X, she wrote: ‘There’s no info or briefing on this. I would not know what to advise a patient. How many 1000s of women will contact their GP today & feel “let down” that “no one knows anything about this”?’
‘What fantastic news, but how incredibly unhelpful to have had zero discussion with GPs? This sort of public messaging is incredibly unhelpful to GPs and frustrating for their patients. Come on, NHS England – it’s a recurrent pattern,’ Dr Bramall-Stainer added.
Dr Selvaseelan Selvarajah, a GP in East London, wrote on X: ‘Great news. Problem is that an overstretched #TeamGP doesn’t have the resources to have these discussions with all the worried patients. Let’s do this properly for patients and fund it.’
Sheffield GP Dr Ben Allen said GPs will now have to assess eligibility, refer and have ‘difficult conversations’ with those who are not eligible – but with ‘no extra resources allocated’.
‘We’ll just do it in our spare time alongside everything else! (& be judged on access),’ he wrote on X.
To access anastrozole for prevention, which is taken as 1mg tablet once a day for five years, patients will be referred by their GP to specialists who can conduct full risk assessments.
According to NHS England, if a quarter of eligible women take the drug, around 2,000 cases of breast cancer could be prevented in England.
Anastrozole is now off-patent, and was first recommended for preventive use by NICE in 2017.
NHS England’s cancer director Professor Johnson told BBC Radio 4: ‘If you’ve got a strong family history of breast cancer, if you’ve got one or more close relatives who’s had breast cancer, particularly if they’ve had it at an early age, this is something to discuss with your GP about whether this might be suitable.’
It is the first drug to be repurposed through a national programme hosted by NHS England, set up in 2021, which seeks to build on the medicines repurposing seen throughout the pandemic.
NHS chief executive Amanda Pritchard, said: ‘It’s fantastic that this vital risk-reducing option could now help thousands of women and their families avoid the distress of a breast cancer diagnosis.
‘Allowing more women to live healthier lives, free of breast cancer is truly remarkable, and we hope that licensing anastrozole for a new use today represents the first step to ensuring this risk-reducing option can be accessed by all who could benefit from it.’
Earlier this year, a UK study found that most women diagnosed with early-stage breast cancer today can expect to become long-term survivors.
Over the summer, GPs expressed concerns about the Government ‘promoting’ unofficial prostate cancer screening on social media.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.
Related Articles
READERS' COMMENTS [9]
Please note, only GPs are permitted to add comments to articles










Why have consultants not been discussing this with all suitable women for the last 6 years? Did they forget?
Well, I can see them getting a lot of referrals into secondary care in the next few weeks now!
great way to cut waiting lists!
Helpful from the Prof.
Risk tools exist (think Manchester) but as already said we GP’s have unlimited amount of free time to discuss this with patients.
Fine. Unfortunately most people dont appreciate just because great aunt Joan had cancer, oesnt put them at risk.
So just another referral into the Genetic Breast screening service – and the waiting lists keep going up!
See GP?
Hahaha hahahaha
Assess eligibility??
Just refer them all.
This is public health not GMS work. If they want GPs to do this they need to fund it as a LES. Usual NHS nonsense of announcing something before briefing doctors. No NICE guidance on this, no thought about capacity, no consideration of need for DEXA scans.
Yet another NHSE fustercluck clown-show…..
-No warning to GPs this was coming
-Info gleaned from some Prof on Radio 4
-no clarity on eligibility…..is “close” family a 1st degree relative? How young is “young”? <50? How many patients precisely know the age their relative was diagnosed at? Wouldn’t they just lie to qualify?
– is it only post menopausal women who qualify? So a 45 yr old post menopausal patient can have it, but a 55 year old still having periods cannot?
– who do we refer to? Breast clinic? Genetics? Do they have the capacity? Is there an algorithm? Guidelines?
-do we expect eligible women to come forward of their own volition, or do we proactively seek them out? Isn’t this the job of Public Health?
– when a desperately worried patient rejected on failing to meet inclusion criteria develops breast cancer, who is she going to blame?
NHSE going for “good news” publicity whilst leaving GPs totally in the dark despite encouraging patients to “see their doctor “ for advice. What a shambles.
Not sure what GPs will add clinically to this, that self referral into breast family history clinics wouldn’t achieve. Apart from who does the work! Also have to consider decent increase in osteoporosis, genital atrophy/ sexual dyfunction created by anastrazole. Will generate quite a few symptomatic menopausal patients who won’t be able to access HRT presumably too.
If NHS tell patients to ask for something that is unfunded and unfamiliar, there will be alot more referals. Do not then blame GPs for the long waits!