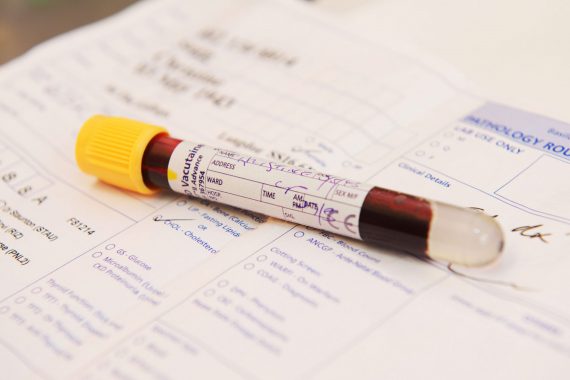
Delayed or missed diagnosis is the number one cause of claims the MDU settles on behalf of GPs. Problems with tracking test results often feature in these cases. These problems can easily be prevented with a few simple tips.
1. Track each stage
There are a number of steps involved in managing test results and at each stage there is potential for results to be lost in the system – from the lab, to the GP reviewing the results, to notifying the patient.
It is important that your practice has a system in place to ensure all of these steps are carried out and a tracking system can help. You might use a paper log, a computer spreadsheet, or specialised computer software to track results, with all requested investigations logged, and then each step checked off when complete.
2. Be consistent and have safeguards
All clinicians and support staff should be using the same system, and it should be clear whose responsibility it is to deal with each step. For example administrative staff should log tests in and out and ensure the relevant GP is alerted when results are received. GPs should review results to decide if action is required and ask the patient to attend for a follow up appointment if necessary.
A safeguard should be introduced so that if a result is not received within a specified time period, the requesting clinician is informed.
3. Get patients involved
Ensure the patient understands what tests you are requesting, and how the results will be followed up. It can help to provide this information in writing, with instructions for the patient on how long to wait before phoning or making an appointment to get the result. It adds another layer of safety to the system if patients are encouraged to contact the practice for results, however ultimately it is the practice’s responsibility to ensure patients are aware of test results needing further action.
4. Report errors
Be aware of errors and mishaps so that your system can be improved if it’s not working. Encourage staff to report errors or near misses, and implement a system for learning and improvement as a result. For practices in England, NHS England has devised an ‘e-form’ to make it easier to submit patient safety incident reports to the National Reporting and Learning System (NRLS), the NHS’s national patient safety incident database.
5. Take full responsibility
If a test result is lost or delayed and the patient makes a complaint, or the mistake is serious enough that it may have contributed to the patient’s death and there is an inquest, then the actions of individual doctors, practice policies and systems could come under close scrutiny. While every case is different, it is generally accepted that the clinician who requests the investigation is responsible for checking the result and ensuring the patient is appropriately informed, rather than placing responsibility on the patient to attend for results. No one wants to be responsible for a lost test result which causes a patient to come to harm, but with the right systems in place, you can minimise the risk.
Dr Beverley Ward is a medicolegal advisor at the MDU
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens