Medicolegal risks and rewards of working at scale
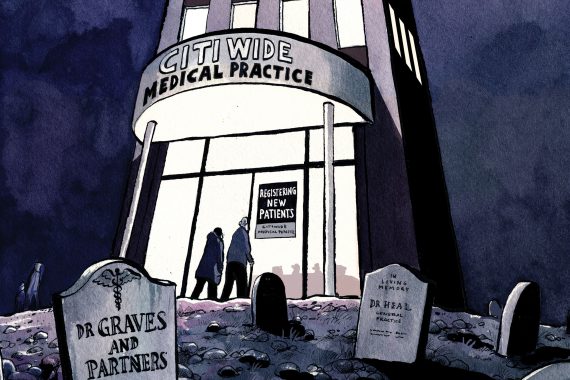
To safely deliver new models of care it is essential that practices adapt their processes and structures. Processes that successfully deliver safe and effective care in a small, single partner practice are not likely to cater to all the risks faced by a practice in a new care model, or working at scale in a group or federation.
Any practice bringing in new roles, such as paramedics, physician associates or pharmacists, will need to have clearly defined scopes of practice and supervision arrangements, and that is just the start.
But there are some rewards too in terms of reducing risks. Here are some of the risks and rewards of working at scale.
Make sure you have patient consent for other practices to access patient records
Where practices join together, either tightly in a formal federation, or loosely in a hub network, it is possible that patients will receive some care away from their usual practice. Safe and effective care from a different practice is more achievable when healthcare staff can access records held by the patient’s base practice, so that they are aware of the patient’s past medical history, medications and any recent attendances. Access to patient records is particularly important when a patient attends another practice with an acute medical problem. Effective collaboration and communication between practices will enable GPs to resume care seamlessly, minimising the delays sometimes seen when patients attend A&E departments or urgent care centres.
Collaboration has allowed some vanguard practices to expand service capacity, including during extended and unscheduled hours. As well as shared records access, effective triage is vital: technology can assist here to prioritise patients by the urgency or complexity of their clinical needs.
You need to obtain patient consent before sharing their records with other practices. Explaining to patients the motives and expected benefits of sharing medical records with partnership practices is likely to help when seeking to obtain patients’ consent to do so.
However, you should remember that GMC guidance (Confidentiality, 2009, paragraphs 25-27) advocates respecting the wishes of any patient objecting to the sharing of particular personal information within the healthcare team, unless disclosure is considered essential for providing safe care.
You need to harmonise induction, training and supervision
Increased collaboration between practices requires consideration of the benefit of harmonising policies and protocols, including the induction of new staff and the training needs of existing staff.
If different staff are following different policies and protocols across practices, there is a risk that patients whose care is shared across these practices might be subject to inconsistent or contradictory approaches, with the potential for inequality in provision, for example if one practice has a different threshold for referral or prescribing.
Staff, especially those working across practices, require clarity regarding their roles, reporting arrangements and resources, including access to supervision. This is especially important for new healthcare roles in primary care, in order to determine professional accountability (as doctors are accountable to the GMC for delegating safely and appropriately). It also assists patients to understand who is treating them and what they can offer.
In terms of accountability, a regulated associate would be accountable for their own actions. However, it is in their employers’ interest to manage the litigation risk associated with their practice.
Collaborating practices can benefit from economies of scale in providing for the training and CPD needs of primary care teams, including ensuring appropriate supervision of any staff subject to regulatory requirements for workplace reporting and supervision.
You can share best practice for clinical administration
Sharing best practice regarding processes and policies allows harmonisation – a good example of which, is handling investigation results. Reducing the risk of failing to act on abnormal results, for example in relation to INR monitoring, PSA testing and renal function testing, is likely to decrease adverse events and have a beneficial impact on complaints and litigation.
Similar benefits are possible from sharing best practice in relation to handling medication reviews and repeat prescription requests.
Hub working can allow more effective complaints handling
As well as helping with the implementation of approved national guidance and the undertaking of audit through shared clinical governance support staff, hub-working provides for effective and objective complaints handling. This is because a practice is able to obtain independent peer reviews of its complaints and significant events from a hub partner. Further, any lessons learned can be shared across the network, allowing central modification of protocols or processes to minimise the recurrence of similar complaints or adverse events.
Dr Helen Hartley is a medicolegal adviser at Medical Protection









