With ever-increasing workload pressures leading to stress and burnout, being able to refer a patient to secondary care can allow GPs a moment of breathing space.
Firing off a referral diverts some responsibility for a while. Someone else is overseeing that patient’s care now – the burden is off me.
NHS England looked set to burst the bubble in the autumn, however, when reports began circulating of a strategy to limit GPs’ scope to make hospital referrals.
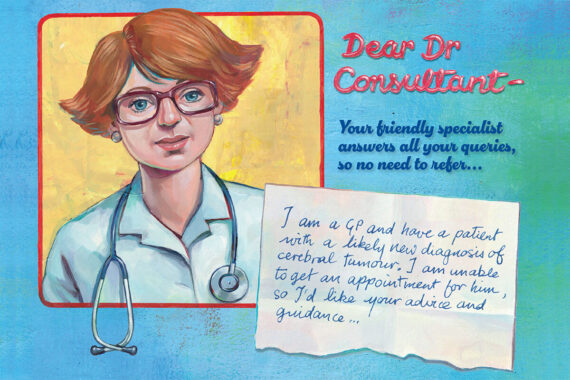
There was talk of significantly reducing the number of referrals to secondary care and increasing the use of advice and guidance (A&G) instead.
Pulse delved into the issue of A&G in October, unveiling the manifold potential problems for GPs and patients alike.
Top of the list is that A&G pathways unavoidably increase the amount of work GPs need to do.
If a referral is rejected and sent back with advice, the onus is on the GP to follow up, often requiring another consultation with the patient and sometimes needing to arrange scans and a barrage of tests.
One GP told Pulse that following an A&G pathway for one patient might take six hours – versus a few minutes to do a referral letter.
It also places pressure on GPs to include more detailed information in the request, as secondary care colleagues only have that information to go on when deciding what advice and guidance to give.
Some GPs may be uncomfortable with responsibility for that, and for retaining clinical oversight of patients who should be under the remit of a specialist.
To rub salt into the wound, consultants are funded to complete A&G requests. GPs are not, save for some in Tower Hamlets, east London, where the LMC managed to secure £19 per A&G episode from the ICB.
There are instances where A&G is creeping in even before it’s mandated. Take the case of neurology referrals in Nottingham, where a new triage system resulted in 40% of GP referrals being rejected or returned, with either requests for more information or with (unsolicited) advice and guidance. Before the system was introduced just 7% of referrals were not seen through.
Overall, the use of A&G in England has increased 60% in the past two years: from 140,000 monthly requests in Q1 2021 to 210,000 by July this year.
And NHS England has signalled its intention to further expand the scheme, pointing to dermatology as an area in which A&G should be the default pathway. In practice, that means GPs are already having to include dermatoscope images with referrals.
GPs say that even when A&G is appropriate and works well, it can take weeks before they actually get back any advice and guidance. Hospital waiting time figures look better, but it pushes the problem back down the system to primary care.
Patients still have to wait, but they’re waiting to hear from the GP instead of from a hospital. Once again, the GP is the fall guy – and that’s exactly where patients direct their dissatisfaction.
As one GP said, ‘it’ll be the GP who’ll be labelled as the bad cop’ because ‘patients can actually put a face to the name of the GP [and] that’s where the complaint ends up – on the GP’s desk’.
Just a few weeks ago, NHS England confirmed to Pulse that there will be no national mandate for GPs to use A&G in a certain number of cases.
This is unlikely to reassure many GPs, who report seeing more referrals landing back in their in-tray with various actions needed, and fielding more questions and complaints from patients.
Mandated or not, it seems A&G is here to stay.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













With advice and guidance, you get effectively an outpatient letter back within one week rather than an average of four months. You might argue this is less work as you’re not having to hold the care of that patient in that time, worry about them, and juggle on occasion multiple referrals with multiple pathology.
In the good old days it was not uncommon for a G.P. to refer a patient to a consultant with a letter saying
”Please see
? chest”
Regards
Revolutionary idea- GP decides if they want A and G or a F2F.
In what world does following an A&G pathway for one patient take six hours for a GP?!