Pulse 2019 review: GP practices face ambulance delays
Patients will probably think that, if they’re going to have a medical emergency, there are worse places to have it than the GP practice.
Surrounded by doctors, you’re in safe hands until an ambulance arrives. Paramedics will surely get to you quickly because, with a trained GP deciding you need an ambulance, they’ll realise this is serious – right?
Well, wrong, as Pulse discovered back in January.
Rather than being at the front of the queue, patients who have the misfortune of needing emergency medical assistance while at the doctors will, in fact, face longer waits.
Because ambulance trusts across the country are deliberately delaying sending blue light assistance to GP practices.
Pulse’s investigation found that, on average, ambulances take more than twice as long to get to 999 calls placed by surgeries than those made by the public or other services – the assumption being that GPs are able to handle things until help arrives.
But that’s not always the case. One GP told Pulse that they’d waited with a patient with sepsis for three hours, during which time the oxygen being administered had run out. In another case, a patient who’d waited 90 minutes for an ambulance had died.
As BMA leaders pointed out, GPs can spot when emergency care is needed, but they’re not trained to provide it.
Yet, from October this year, all healthcare professionals requesting emergency help will have to score a patient’s medical need based on an assessment of six vital signs: respiration rate, oxygen saturation, systolic blood pressure, pulse rate, level of consciousness or new confusion, and temperature.
Understandably, there’s deep concern that this could put patients at risk.
If ambulance trusts are already downgrading calls from practices as standard – the presence of a GP and a defibrillator is sufficient to meet some government targets – then it’s hard to see how scoring a patient’s vital signs will speed things up.
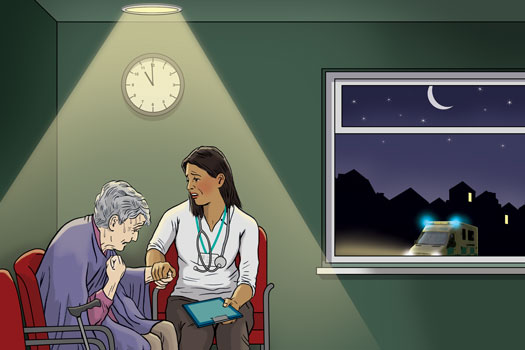
Not to mention the burden that places on GPs, as they find themselves in the unenviable position of sitting in the consultation room with their seriously ill patient, watching the minutes tick by as their condition deteriorates.
Now they have to justify their decision to call an ambulance.
This was illustrated poignantly by Kent GP Dr Mark Ironmonger, who’d witnessed a life-threatening emergency at a restaurant and sprang into action. Despite telling the ambulance dispatcher that the patient was possibly in the midst of a third MI, there was an 80-minute wait between the first 999 call and the paramedics arriving.
‘In the meantime, I’d been left in charge of a life-threatening situation unsupported, equipped only with a set of cutlery, drinking straw and my fingertips,’ Dr Ironmonger said.
‘Despite doing my best to reassure the patient and his relatives throughout, this was a highly distressing scenario all round.’
It’s no surprise that some GPs have resorted to having the patient’s relative call the ambulance, believing they’ll get a speedier outcome.
In a life-or-death situation, asked whether there’s a doctor in the house, it seems the best response is a firm ‘No’.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens











