Is Cancer Research UK’s obesity campaign ‘fat shaming’?
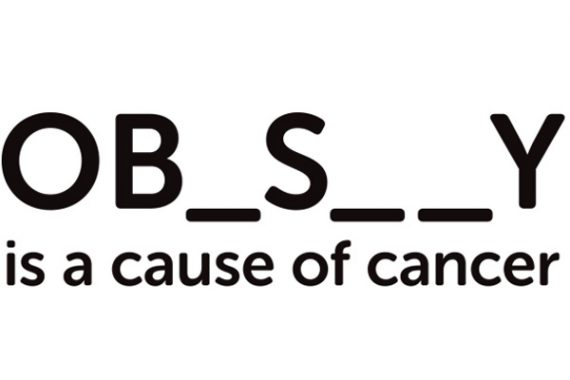
Picture: Cancer Research UK
Cancer Research UK has generated controversy with a new publicity campaign that explicitly links obesity with cancer. Does the campaign – including posters evoking public health warnings and cigarette packets containing chips – amount to ‘fat-shaming’ as critics say? Two GPs debate the issue for Pulse.

Yes. This only serves to stigmatise obesity further
It is a commonly held moral trope that fatness is a punishment for the twin sins of gluttony and sloth. Punishment for the aesthetic crime of publicly displaying a fat body is that of mockery, shaming and disgust. Now that fatness has been medicalised as obesity, people who are obese are additionally guilty of being a burden on the NHS and the economy.
When this public stigma is internalised and the moral opprobrium is internalised, the consequence is shame. Shame is an inner voice that says, ‘I’m disgusting’, ‘this is my fault’, ‘I deserve this because of who and what I am’. This contrasts with guilt, in which it is possible to separate the deed from the person.
Common sources of shame in patients who confront medical professionals include mental illnesses, incontinence, disfiguring conditions, poverty, ignorance and dependency. For someone who has been obese since childhood, who sought or seeks comfort in food, because the rest of their life is so insecure, any sense of agency is severely impaired. The ineffectiveness of weight loss interventions and the links between shame, stigma and weight gain prove this.
If the Cancer Research UK (CRUK) adverts are intended simply to state a fact – ‘you’re fat and you’re going to die from cancer’ – but not to provoke action, then it will have achieved nothing. So we should assume it is intended to provoke change; either to encourage obese people to get tested for cancer or to encourage obese people to lose weight.
Shaming people has been shown to make them do more self-harming behaviour
But the charity should know better than anyone that telling smokers they were going to die didn’t work – it was legislation that cut smoking rates. And obesity is far more complex than smoking – you can’t put a ban on eating.
Shaming people has been shown to make them do more self-harming behaviour to compensate for the distress. Indeed, behaviours in children and adults that have experienced significant adversity are often compensating for, or dissociating from, feelings of shame and fear. They include obsessive-compulsive rituals, sexual proclivity, drug and alcohol abuse, social isolation, self-harm and eating disorders such as comfort eating. The first study to show the long-term effects of childhood adversity was in an obesity clinic and found strong links between childhood sexual abuse and severe obesity. These links, while widely researched, are not part of medical education, which partly explains why doctors’ stigma and bias towards overweight patients is as prevalent as it is among the general population.
What then should CRUK do? Rather than shaming people, which we know risks causing them to eat more and withdraw from care, the charity should seek to empower them. It should shift the focus of attention onto the obesogenic environment, rather than obese people. And it should put more effort into informing and educating policy makers and the public about the links between inequality, lifestyle and cancer.
The current approach is simply reinforcing stigma and risks doing more harm than good.
Dr Jonathon Tomlinson is a GP trainer in east London
Further reading
Vartanian, L and Porter, A. Weight stigma and eating behaviour – a review of the literature. Appetite; 2012: 102: 3–14
Tomlinson, J. Shame. A Better NHS; 2012
Tomlinson, J. Doctors, patients and obesity. A Better NHS; 2011
Scrambler, G. Weaponising stigma. Author’s blog; 2018 http://www.grahamscambler.com/weaponising-stigma/
Stevens, JE. How the adverse childhood experiences study began in an obesity clinic. Aces Too High; 2011
On being a fat medical student, at the start of our metabolism module. Raspberry Stethoscope; 2017
Sample, I. Fat to fit: how Finland did it. Guardian; 2005

No. The public deserves to know the truth
Fat shaming and size discrimination is devastating and hugely damaging to people. I have patients who have been overlooked at work because of their size, abused by partners for being overweight and openly discriminated against in social circles for being too large.
So why am I not upset or offended by the most recent Cancer Research UK (CRUK) campaign highlighting obesity as a major cause of cancer?
Because, quite simply, this is not fat-shaming, but fact stating. This is not a charity’s pejorative judgment of body idylls and aesthetics. We mustn’t let the perennial desire to be offended get in the way of awareness-raising and good health education.
In data published by CRUK, only 15% of people knew obesity to be one of the major causes of cancer; yet it is the second biggest cause after smoking. The correlation has been evident since the 1970s but at that point cause and effect was not definitively established.
Has it ever been offensive to point out smoking is dangerous?
Now a huge body of high quality data has established that obesity is a cause of some 13 cancers, and revealed a dose-response relationship between the degree of obesity and level of risk. The data are high quality, with confounding factors accounted for: as you would expect from our leading cancer charity. The current national advertising campaign was piloted two years ago with its value verified before it was nationally rolled out.
Once CRUK had this body of optimal scientific evidence should they have hidden it from the public to save offending people? As a GP, a patient, a parent and a journalist I feel the ‘fat-shaming’ allegation against CRUK is a case of ‘political correctness gone mad’.
I am involved in the current Be Clear on Cancer campaign talking about breast cancer risk in the over-70s. Is that ageist? After all, women don’t choose to get old. Are the adverts targeted at BME groups regarding prostate cancer racist? Of course they’re not – they raise awareness among specific populations who deserve to be educated by truth.
Importantly, the aim is not just to educate individuals but also government, industry and policy makers. Publicising this factual message, enforces appropriate lobbying power and influences strategy, adding pressure on companies to lessen obesity in children through sugar reduction policy and responsible marketing.
An argument levelled against the CRUK campaign is that people don’t choose obesity and pointing it out somehow blames the individual. I agree, but similarly people do not ‘choose’ smoking – they became smokers through experience, cultural influence, trauma, their social environment and many other factors. Has it ever been offensive to point out smoking is dangerous? No, of course not, it is merely factual health education.
What do we want our leading cancer charity to do? Raise some money and say ‘there, there’? No, this is what our cancer charities should be doing. Putting tough messages into the public domain to inform, drive awareness and save lives. I am proud as a British doctor that CRUK runs campaigns like this to help individuals, government and stakeholders beat cancer.
Dr Ellie Cannon is a portfolio NHS GP in London and broadcast media doctor
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









