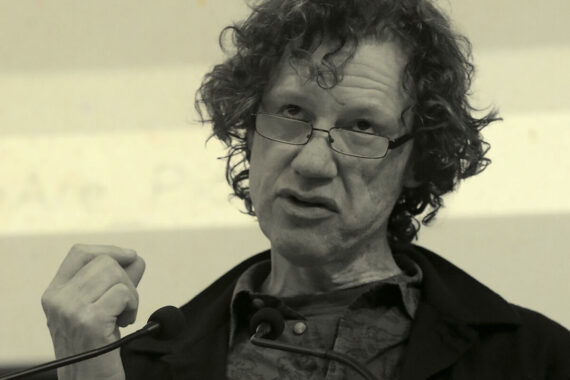
In a special feature, satirist Chris Morris – the son of two GPs – follows his star turn at the 2023 LMCs conference with a piece for Pulse on the Government’s destruction of the NHS and general practice
I grew up in a GP household where Pulse lurked in the paper pile. You want National Geographic’s pictures of the moon landing? Have some photos of burst skin; purple or suppurating, often both and inside the mouth. I grew up listening to doctors – the voices that lulled us with bedtime stories also said words like thrombosis and pneumothorax. Absorption bred mimicry, so for the past 35 years I’ve provided GP services to a growing number of loyal patients who have no idea I know nothing whatsoever about medicine.
Alright I haven’t. I couldn’t do the work of a GP. Unless I joined Operose as a physician associate.1 That’s not a cheap joke. It’s a false-economy joke. It’s not a PA’s fault the Government wants them instead of qualified doctors, or that it has allocated £1.4bn to pay for GP staff but only for additional roles, not doctors.2 More doctors and nurses would provide more appointments and better care for less money.3 Its not the PA’s fault ministers would rather attack GPs than listen to them.
The Government drives GP numbers down by making their lives impossible.4 It berates them as lazy when they’re seeing more patients than ever and vaccinated most of us in the pandemic. In 2015, Jeremy Hunt promised 5,000 more GPs by 2020. We’ve ended up with 2,000 fewer. Johnson trumped Hunt and promised 6,000 but the poor man can’t speak the truth unless he’s using it to tell a lie so let’s leave him in his padlocked wheelie bin hiding from daylight like a killer toad licking the guilty sweat off its belly and deleting its WhatsApps.
Politicians duck blame and tell their friends in the press to vilify doctors. Does it work? Our satisfaction with the NHS has never been lower5 but who do we think is responsible? That same survey shows a marked increase in satisfaction among those who actually see someone. In other words, we trust the people who look after us more than politicians and their executors, even if we don’t know exactly who they are. NHS England sounds like the organisation that looks after you when in fact it is an executive body dreamt up by Andrew Lansley to shield himself and future health secretaries from direct responsibility for their own job. NHSE was called the Health Commissioning Board before it rolled itself in glitter.
The way forward is not mysterious. The recent Health Select Committee report on the future of general practice prescribed increases in recruitment, retention, funding and continuity of care.6 Committee chair Jeremy Hunt supported the plan but, as chancellor, has failed to back any of it. But its recommendations are widely appreciated – by the BMA and RCGP, GPs like Helen Salisbury and the indefatigable Steve Taylor, GP researchers like Becks Fisher, Phil Whitaker in his excellent book What is a Doctor? and many more. Common themes abound. Money spent upstream goes further. Primary care should receive more than 8% of NHS funding. Boost retention, don’t undermine it.7 Support partnerships, they work. Yet against its own advice, the Government refuses to issue new partnership contracts even though private provider practices are worse for patients.8
Practices in deprived areas need more money, so abolish Carr-Hill and fund them properly. And let’s throw in the Marmot Report (and its update) and fix housing, poverty and public health. These are all broken and affect health outcomes far more than anything the NHS can do. Ignoring our poor public health is an easy way to make the NHS look worse than it is. Remember this next time the media offers you that absolute Think Tanker Kate Andrews.
Is restoration of general practice an impossible dream? Is the practice so wonderfully described in Polly Morland’s A Fortunate Woman a rare exception? My conversations with practices in deprived areas suggest not. In a few, patients still have a named doctor and continuity is strong. Others aspire to this but are overworked and bogged down by admin. Good practice depends on resources, support and, yes, money.
Finding money doesn’t have to mean cuts. NHS 111, for example, offers advice from people even less qualified than me reading NHS Pathways off a screen. Like the Babylon doc-bot (RIP, boohoo) they can’t tell tennis elbow from a heart attack so err on the side of caution. This means 25% of 111 calls are referred to A&E. When GP co-ops took the calls, it was 1%-2%.9 An A&E visit costs 10 times more than seeing your GP. Continuity also reduces costs and can increase your chances of staying alive by 25%.10 Properly supported, the family doctor works almost like magic.
This spavined Government refuses to act on any of this. Will Labour do any better? We need a health secretary prepared to ignore lobbyists bent on forcing untested drugs like Inclisiran into us: Novartis lobbied Government, which bullied NICE into fast-tracking the drug; GPs said ‘hang on a minute’.11 Ministers should ignore management consultants who know nothing about healthcare, charge millions for their ignorance and cost more than they save.12
We need someone who listens to doctors, like the ones I met at an inner-city practice with a high-stress list. It’s a place you’d expect to be struggling but it thrives on a continuity of care ethos that puts patients first. There’s no 8 o’clock rush – you can book any time of day and all appointments are face to face. One way they achieve this is to negotiate hard with their ICB to keep the practice from expanding to a size that would break their system.13 If new housing goes up, start a new practice.
A visiting Labour policy adviser praised their model of general practice as ideal but suggested it wouldn’t win an election. What?! Access, continuity and a practice rule that the phone never rings more than three times and is answered by a human being? Who wouldn’t vote for that? At the time of course, Labour had decided they were very much against partnerships and Wes Streeting was spouting nonsense about ‘self referral’ and ‘tearing up GP contracts’ and putting them all on salary. So the adviser’s schizoid flip was consistent with the boss’s ravings.
Since the fracas of January 2023, Labour have learnt to say they are now in favour of the ‘family doctor’ but they have not specified what that means, let alone make a manifesto commitment to partnership practices and complete continuity of care. Since this article was originally printed Labour have perhaps not surprisingly tried to insist that Pulse change the copy in relation to their policy on general practice. Instead, I’m happy to confirm that this has flip-flopped in the last 12 months without showing any sign of stabilising. I note they have yet to make a manifesto commitment to the sort of general practice that demonstrably works and which an overwhelming majority of voters (of whom GPs see 1.4 million per day) want to see returned to them. Instead there are signs Labour intend to perpetuate the Tory sponsored blueprint of NHSE which blocks its ears to GP knowledge and issues commands based on metrics and ignorance.
In the mid-1960s, general practice was dying. My parents’ income didn’t even cover their standing orders. The 1965 Family Doctor Charter called for a revolution in funding and the resulting contract reversed the problem. Sure, money’s tight now, since Liz Truss and the Institute of Economic Amateurs flushed us down the Kwasi. But we should beware the sirens of austerity who slashed public health, binned our PPE stockpiles, and sacrificed us and our NHS to Covid. In 1948 our broken economy didn’t stop us establishing the NHS. We can fix it now without blowing the bank. Every pound invested in the NHS delivers four pounds back into the economy.14
Wes Streeting plans to spend more on primary care to relieve hospitals. That’s good if he heeds doctors’ advice on how to spend it. They’ll tell him he won’t have to choose between continuity of care and access, he can have both.15,16 Bottom-up decision making works better than top down.14 Ignoring doctors is a wrecker’s game and an attack on every single one of us.

References
- BBC. UK’s biggest GP chain replacing doctors with less qualified staff. Jun 2022. Link
- Pulse. Thousands sign petition asking for GPs to be included in ARRS. Jan 2022. Link
- X @iDrSunny. The productivity of GPs outstrips the roles being used in primary care. Nov 2023. Link
- The Health Foundation. UK GPs suffering unsustainable workplace pressures. Mar 2023. Link
- The King’s Fund. Public satisfaction with the NHS and social care in 2022. Mar 2023. Link
- Health and Social Care Committee. The future of general practice. Oct 2022. Link
- RCGP. ‘We need to expand retention initiatives; not stop the ones we have.’ Jan 2024. Link
- Cowling C et al. Contract and ownership type of general practices and patient experience in England. J R Soc Med. 2017;110:440–451. Link
- Phil Whitaker. How to save the NHS. New Statesman, Jan 2023. Link
- Sandvik H et al. Continuity in general practice as predictor of mortality, acute hospitalisation, and use of out-of-hours care. BJGP 2022;72 (715): e84-e9. Link
- Cohen D and McCartney M. Inclisiran: the ‘extremely unusual’ political influence behind the novel drug’s approval. Pharmaceutical Journal, Dec 2023. Link
- The Conversation. Management consultants don’t save the NHS money – new evidence. Feb 2018. Link
- Edwards P. Bigger practices are associated with decreased patient satisfaction and perceptions of access. BJGP 2022;72(722):420-421. Link
- Taylor M. A more ambitious national social contract for healthcare. RSM, May 2023. Link
- The Health Foundation. One care: continuity of care evaluation report. June 2021. Link
- Nuffield Trust. Improving access and continuity in general practice. 2018. Link
Please note, this article was amended at 9:20 on 23 February to reflect that the individual who visited the inner city practice in London was a Labour policy adviser, and not a SpAd (special advisor). It was later amended at 11:45am on 27 February to include context around the SpAd’s visit
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












Mr Morris thank you. Love your work!
Brilliant and passionate, thankyou.
Excellent. all so true. So tragic that money has been spent on “add ons” all these year and not on the core of what we do. Divide & rule innit?
Excellent article and very accurate
The government seem to only listen to sycophants and seemed determined to destroy the NHS
Entirely agree deprived areas need realistic funding
This is where most improvement to health occurs per individual
Very good article
Absolutely right. The government could start with something completely free & would make themselves look good and increase respect for our hard working GP teams by positively promoting general practice. Tell the voter how well we’re doing, under difficult circumstances and how incredibly cost effective we are. How we are an accessible service with free, bespoke one to one consultations with experienced health professionals- where else to you get that? How the UK is lucky to have such a brilliant service who is protecting our population from the deteriorating hospital services and unavailability of holistic secondary care. Addressing the tidal wave of lifestyle disease would rapidly improve population health & could be done without taking from the NHS budget. Lifestyle conditions & self limiting illnesses must be the cause of over 90% of the illness we see. Why couldn’t this be funded this from regulating food companies, giving evidence based messaging to the country promoting self management & personal responsibility. , Promoting exercise & activity. Educating our population before they make themselves ill. Employers to address unhealthy & stressful working patterns etc. it’s not too late for this & there could be measurable benefits within a few months – but inaction will cause the NHS to continue to implode until it is just a distant memory…..
Fantastic and so well researched.
Please Please could you do this on the mainstream telly Chris? It worked for the poor post office guys.
Indeed Ian Morris, a Day Today style satirical clip for YouTube would help to highlight the absurdity and idiocy of government and NHSE decision making dogma.