Treating patients with Ebola in Sierra Leone

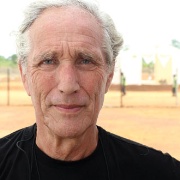
Profile Gordon Gancz
Age Over 65
Role Volunteer in Port Loko, Sierra Leone, under an NHS scheme. Usually a GP and senior lecturer in Oxford
Location Port Loko, Sierra Leone
07.00
I wake up in my own room and eat a bowl of cereal. I hope the milk hasn’t gone sour; the people who run the staff accommodation turn the generator off at night to save power and during the day the fridges warm right up – temperatures can reach 32°C here.
I’d never worked abroad before this, but I’ve stayed in army accommodation as a civilian adviser to the armed services. But unlike that experience, most of the time the shower here doesn’t work, and the laundry service brings your clothes back smelling worse than when you sent them.
08.00
I have a meeting with heads of department to plan the day, then make the three-mile trip through the bush to the Ebola treatment centre (ETC). It’s called a ‘treatment’ centre, but as there’s not yet a cure, all we can do is keep patients rehydrated (as per WHO guidelines). I am responsible for staff health so I travel in an ambulance fitted to treat both Ebola and non-Ebola illness, including traumas (there’s a high risk of road accidents here).
09.00
Arriving at the ETC, I begin the elaborate handwashing routine. It certainly lays to rest any anxiety I had about the infection control part of CQC inspections. We use some of the operating procedures we developed in York where we trained (casualty evacuation plans, for example), but others we adapted when we came over. I also take my temperature because I’ve established a practice where no staff member with a temperature over 38°C is allowed inside in case of ill health (such as malaria, Ebola, or a stomach upset).
But when you’re dressed up in an Ebola suit and two masks, goggles, a snood hood, a rubber apron, wellington boots and two pairs of gloves, you get incredibly hot. Just yesterday, a member of staff came out of the red zone (where Ebola patients stay) having been in for an hour instead of the recommended 35-40 minutes. He collapsed, so I had to resuscitate him – undress him, spray him down, get his legs in the air, try to restore his blood pressure and pump him full of rehydration salts in the hope he didn’t fit.
In the red zone, we use a buddy system to watch out for one another. We also write our names on our suits so patients and colleagues know who’s inside them.
We currently have 12 patients, but this will go up to 20, then 100 when we operate at full capacity.
14.00
Twenty new doctors arrive from Denmark, who will take over from us when our stint ends. I explain our systems, what their lives are going to be like and give them top-up training about protective equipment. Then they start shadowing us in the red zone.
15.00
As the lead for staff health, I have a very varied workload. For instance, yesterday I saw an impacted wisdom tooth, secondary syphilis, appendicitis and a patient who had jumped off a moving bus. I also visit the government hospital to diagnose and prescribe for patients discharged from the ETC. Many survivors have other health problems after Ebola, such as the nine-year-old girl who is now being treated for bilateral pneumonia.
17.00
I visit the Command and Control centre with the police commander, a colonel and the local Royal Army Medical Corps leader. We collate key data, such as the number of people who’ve been picked up that day, the number of dead, the number of positive tests and the burial report.
19.00
After consultations with sick staff, I eat supper. I don’t miss English food that much but I can’t deny I was pleased to receive the coffee and Stilton that my son and daughter posted to me for Christmas.
20.00
A four-day lockdown has just begun to keep people off the roads while the army and police go door to door to find people with Ebola-like symptoms. They’re trying to stop the virus spreading – many are reluctant to seek treatment. A lot of people get infected after washing dead relatives before burial – whole families have been wiped out in this way.
00.00
I go to bed, but I’m on call and have had to deal with something every night so far – thankfully just over the phone.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.



 Oviva’s fully remote Tier 3 Weight Management programme
Oviva’s fully remote Tier 3 Weight Management programme





