Exclusive CCGs are costing thousands of lives and contributing to poor care by not providing GPs with access to faecal occult bloods testing in line with NICE recommendations on colorectal cancer, the GP behind NICE’s guidance has said.
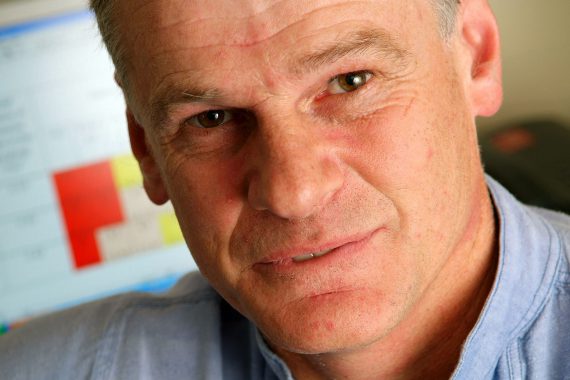
Professor Willie Hamilton, a GP in Exeter and clinical lead of NICE’s guideline development group for suspected cancer guidance, said that there was a lack of access to these tests due to CCG budget pressures, labs’ reluctance to accept large numbers of tests from GPs and a ‘lingering suspicion’ that NICE got its cancer risk thresholds wrong.
He told Pulse that CCGs have been ‘poisoned by surgeons’, who have dissuaded commissioners from funding faecal occult blood testing (FOBT) and faecal immunochemical testing (FITs), arguing that they are not as effective as colonoscopy.
As a result, some patients are needlessly being given colonoscopies while others – who would benefit from FOBTs and FITs – are being left with nothing, he said.
Under NICE’s 400 page long guidance on cancer diagnosis and referral, FOBTs should be used for patients with a risk of colorectal cancer with a 1% to 3% risk, such as those with symptoms such as mild anaemia, with those above 3% having direct access to colonoscopy.
At a Pulse Live event in Birmingham this month, a delegate said they were unable to access for FOBTs for at-risk groups and asked what should be done.
Professor Hamilton replied: ’I think you’ll have to say to them “medico-= legally you’re in deep trouble”, honestly, because there are patients dying in this country.
‘If you request a faecal occult blood and they say “we’re not going to do it” you’re going to have to say to them “I presume you’ll therefore be interested in a letter from the MDU whenever one of my patients is admitted as a bit of an emergency”.’
He added it didn’t matter whether FOBTs or FITs were offered, but one of them had to be offered as an option for patients who didn’t qualify for colonoscopy.
By not doing so, CCGs and labs were ’contributing to poor care’, he said.
He said: ’They’ve of course been poisoned by the surgeons. The surgeons believe colonoscopy is better than FOBTs, they’re right, but FOBTs are better than nothing. Therefore, in a patient group who would get nothing, a FOBT or a FIT is entirely sensible.’
He added that: ‘At least a quarter of this group are being listed for colonoscopy even though they don’t fulfil the colonoscopy requirements in the NICE guidance, and [by implementing the guidance] the CCGs can save pots of cash, patients can be diagnosed early, and we can save a thousand lives.’
Professor Hamilton later told Pulse that there was ’a lot of slowness re FIT/FOB testing with lab reluctance’, and this was partly due to a ’lurking suspicion NICE got it wrong – which we didn’t’.
He added: ‘Other pathway changes to direct tests are slow because it takes time, and most CCGs are under severe financial pressure, with the tangible financial rewards of avoiding emergencies etc not immediately visible.’
In the opening session of the same Pulse Live event, a panel of leading GPs had criticised the disconnect between NICE guidance and the realities of practise. Dr Dermot Ryan, an honorary clinical fellow at the University of Edinburgh said: ’NICE is increasingly irresponsible in not identifying resources necessary to implement the recommendations it makes, they say “it’s not within their remit”, and I think that’s just ducking the bullet.’
And Dr Zoe Norris of the action group GP Survival said that the size of new NICE guidelines left GPs ‘practising in ignorance’ and vulnerable to legal challenge.