Two months ago, a coroner ruled on the death of nine-year-old asthma patient Michael Uriely, finding that 11 chances to save his life had been missed.
Coroner Dr Shirley Radcliffe took the unusual measure of issuing a ‘Regulation 28’ report – which compels NHS England to prevent further such deaths.
Her conclusion was damning: ‘Since the death of Michael Uriely there have been at least a further seven child deaths in London due to asthma and certainly many more throughout the NHS [in] England.’
Indeed, the picture is even worse than that: the number of preventable deaths is rising and the UK has the highest number of preventable childhood asthma deaths in Europe and the third highest in the world.
Given these worrying statistics, have the efforts of the health authorities in been focused on preventing these avoidable asthma deaths?
Sadly, it appears this is not the case. The National Review of Asthma Deaths (NRAD) 1 recommended action on preventable mortality three years ago, but experts say little has been done to implement its advice.
GPs blamed
Instead, attention has focused on GP overdiagnosis, with NICE publishing controversial new guidelines in 20152 recommending the use of a raft of new tests, including FeNO, bronchial challenge testing and spirometry to diagnose the condition.3
The institute claimed that up to one-third of asthma patients have been mislabelled and GPs were accused of trivialising the disease, with some saying inhalers had become ‘almost a fashion accessory’.4
NICE’s radical approach prompted an outcry from the profession. GP experts warned it was ‘dangerous’ to put out a message that so many people diagnosed with asthma may not have the condition, adding that spirometry and FeNO testing would increase costs and workload for practices and mean more referrals to secondary care for extra tests.
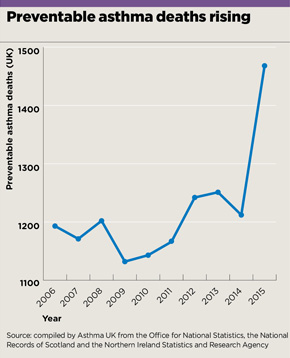
preventable asthma deaths graph may 2017
And these concerns proved prescient. Two years on, the guidelines remain unpublished, appearing to have done little more than complicate matters. NICE took the unprecedented step of pausing the publication of the final guideline to carry out a ‘feasibility pilot’ between May and October last year, which saw 26 practices each given £3,000 to collect data for evaluation, as well as funding for new FeNO kits and any necessary training and extra nurse time.
NICE has so far refused to release the results of this pilot, but Pulse understands they did not go well. The Primary Care Respiratory Society (PCRS) says: ‘Our concerns were borne out in practice, with FeNO found to be expensive, and spirometry time consuming and largely non-contributory to diagnosis in the primary care setting.’
NICE has not denied such reports and has agreed to a second round of consultation in the summer, at which point a full report on the pilot results will be made available to stakeholders.
At the same time, the other pillar of NICE’s asthma revolution – draft guidelines on the management of the condition – is also under fire. Under the proposals, GPs would be expected to offer a course of leukotriene receptor antagonist (LTRA) tablets to patients whose asthma is poorly controlled with a low-dose inhaled corticosteroid (ICS), instead of stepping up therapy by adding a long-acting β-agonist (LABA) – usually done with a combination LABA/ICS inhaler. NICE argues the benefits of LABA/ICS are ‘marginal’ and that trying LTRA tablets rather than going straight to a combination inhaler could save ‘tens of millions’ of pounds a year.
Both the PCRS and the RCGP have rejected this idea, warning it could lead to patients neglecting their steroid medication – and potentially increasing the risk of an acute exacerbation. In its official response to the consultation, the PCRS went as far as to say: ‘This could cost lives if people stop using their ICS inhaler in preference for taking a tablet.’
Dr Duncan Keeley, GPSI in respiratory medicine in Oxfordshire and PCRS policy lead, says there is a consensus forming that NICE should simply drop its plans on asthma altogether: ‘There is a strong sense in the primary care community we would like to go back to one coherent, comprehensive four-nations guideline.
‘We have a long established BTS-SIGN guideline5, which was NICE approved. Our members certainly feel it would be good to have one consistent guideline and there is an intrinsic problem if two authoritative guidelines are saying different things about how you go about diagnosis and management.’
More importantly, NICE’s intervention is an unwelcome distraction from the real asthma challenge: reducing avoidable emergency admissions and deaths.
The national review, carried out by the Royal College of Physicians at the behest of the Government, made a series of recommendations to ensure evidence-based care is properly resourced and implemented across the UK.1
These included GP practices urgently reviewing asthma control for any patient who has been prescribed more than 12 reliever inhalers in a year, every GP practice having a named clinical lead in charge of training staff to manage acute asthma, and all patients having a personal asthma action plan detailing their triggers and explaining when to seek help in an emergency.
And following Michael Uriely’s death, NHS England has been ordered by the coroner to provide details by 19 May about action to implement the NRAD’s recommendations. If no action is to be taken, it must explain why.
The coroner found that Michael’s lung function (peak expiratory flow or spirometry) was not always measured when indicated, his medication was not optimised despite poor control, the frequency of use of relievers was never recorded and he had no personal asthma action plan.
She concluded: ‘I am of the firm opinion that if the recommendations of the National Review [of] Asthma Deaths, published in 2014, had been locally disseminated and implemented [this] would have prevented the death of Michael Uriely.’
NHS England says it is ‘in the process of drafting its response’ to the coroner’s report. But charities are calling for a taskforce on respiratory conditions, which – according to the British Lung Foundation – should look at the controversy over NICE’s guidance.
Dr Mark Levy, a GP expert in Harrow who was the clinical lead for the NRAD report and gave evidence at the inquest, tells Pulse that the NICE guidelines should be ditched. ‘Writing more guidelines is not the answer,’ he says. ‘What we need is a national directive to implement the 19 recommendations in the NRAD… I hope the NICE guidance is scrapped, it is just a waste of time.’
National review: what needs to improve?1
- There should be a designated lead for asthma in every hospital and GP practice
- Patients to be referred to specialist if they have had more than two courses of systemic steroids within the previous year
- Patients to have a written personal asthma action plan and an annual review by a trained healthcare professional
- All asthma patients who have been prescribed more than 12 short-acting reliever inhalers in the previous 12 months should be invited for urgent review
- Routine assessment of inhaler technique and continual monitoring of adherence to inhaled steroids
- The use of combination inhalers should be encouraged
References
1 RCP: Why asthma still kills, 2015. tinyurl.com/NRAD-report
2 NICE. Asthma: diagnosis and monitoring of asthma in adults, children and young people; draft guideline, 2015. tinyurl.com/asthma-draft
3 Pulse Today. ‘NICE: GPs should use FeNO and “twitchiness” tests to confirm asthma diagnosis.’ January 2015 tinyurl.com/mndyfab
4 Bush A, Fleming L. Is asthma overdiagnosed? Archives of Disease in Childhood, online April 2016
5 BTS/SIGN. British guideline on the management of asthma, 2016. tinyurl.com/BTS-SIGN











