Prescriptions of opioids have massively increased in recent years – but there is a growing move to reverse this trend.
Pulse can reveal the BMA has written to health ministers and the House of Commons health select committee calling for an inquiry into drug dependency.
At the same time, the RCGP lead for pain has the support of a parliamentary group for his proposals for annual GP reviews of patients on opioids.
Critics argue there is limited evidence that opioids are effective in chronic pain and the risk of dependency and adverse effects is well documented. But concerns persist over whether GPs have the resources available to offer alternative treatments.
NICE’s latest guideline on back pain advises GPs not to offer opioids routinely for acute low back pain, only to consider weak opioids when anti-inflammatories are not an option, and not to consider opioids at all for chronic back pain.
The Opioids Aware guidelines2 – funded by Public Health England – and the BMA’s Chronic pain: supporting safer prescribing of analgesics,3 published in March, have continued the move away from opioid use, with both stating there is little evidence that opioids are useful for long-term pain. The BMA report cited research that found less-experienced GPs were more likely to prescribe opioids.
Dr Steve Brinksman, a GPSI in pain in Birmingham and clinical lead for the Substance Misuse Management in Group Practice network, explains: ‘The problem is opioids work for less than 20% of people with chronic pain but 80% of prescriptions that get started don’t get stopped.’
But Pulse has learned this could change, and GPs could be in the firing line.
A BMA spokesperson tells Pulse: ‘We have asked the select committee to hold an inquiry into prescribed drug dependence. We had written to former minister for health Nicola Blackwood to discuss this.’
And RCGP clinical lead on chronic pain Dr Martin Johnson says he is in ‘high-level’ talks with decision makers on the issue.
The Sheffield GP tells Pulse: ‘There have been several recent reports on dependency, which raise some good questions, but the issue needs to be addressed at the next level up, with government. So, we’re preparing a high-level inquiry.’
Dr Johnson is in talks with the All Party Parliamentary Group (APPG) on drug dependency. He is in favour of GPs doing annual reviews for all chronic pain patients on opioid drugs. He says this proposal was raised in a 2015 report from the Chronic Pain Policy Coalition,4 which he chairs.
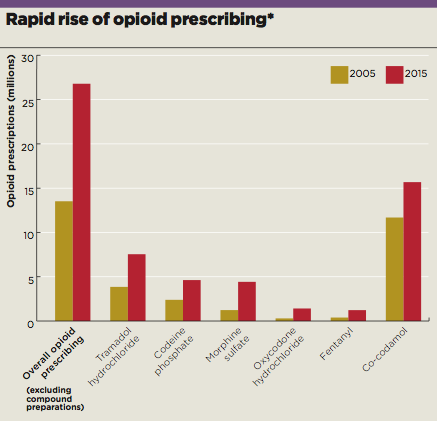
Opioid figures box, July 2017
Poor review process
‘Chronic pain is the largest symptomatic long-term condition, yet we have never had a system to assess people with it,’ Dr Johnson says. ‘People don’t realise that chronic pain is often independent of the reason it developed in the first place.’
Although patients with chronic pain do receive reviews, Johnson says the process is not well defined; it doesn’t have a QOF indicator like asthma or diabetes for example, and a Read code was only introduced in October 2015.
And it seems he has the support of the parliamentary group. Harry Shapiro, director of online advice site Drugwise.org and spokesperson for the APPG, tells Pulse the group would ‘absolutely’ support ongoing monitoring of patients’ opioid use. He had told the APPG meeting last October 2016: ‘We are in the midst of a public health disaster, which is killing hundreds of people a year and ruining the lives of millions.’
The backlash against opioids in part follows recent studies revealing that patients can experience cognitive impairment and hormonal side-effects. Rates of harm have been directly correlated with dose.5
There are also growing concerns over addiction and overdose, following recent trends in the US, where two-thirds of all deaths from overdose in 2015 (33,000 in total) were from opioids.6
Annual reviews may be some way off, but the Opioids Aware guidelines recommend treatment reviews ‘at least’ every six months. The BMA’s report takes a slightly more realistic position, stating only that analgesic use should be reviewed ‘regularly’. It acknowledges the pressure on GPs and recommends that ‘sufficient investment and resources for primary care, including longer consultation times, are required to support improvements in analgesic prescribing for patients with chronic pain’.
And Dr Johnson suggests the burden may not fall solely on GPs. ‘GPs would not necessarily need to do this. There’s a lot of work to suggest that community pharmacists could do it, for example. Plus, many GPs already perform annual opioid checks, we just need to give it a structure.’
But for some, prescribing outside GP practices makes the problem worse. Dr Brinksman says: ‘A lot of the prescribing modalities pain clinics use do cause issues for us. Many will often prescribe neuropathic painkillers, like pregabalin or gabapentin. Although those are useful to some patients, they are open to abuse too.’
The BMA GP Committee’s prescribing lead Dr Andrew Green is sceptical about the need for reviews every year. He says: ‘Individual patient circumstances vary so greatly it is unusual for a specific review interval to be appropriate to everyone.’ He also suggests GPs need more resources if there is to be a change in prescribing patterns.
‘Services need to be provided to allow GPs to manage patients in a way that is less reliant on prescribing.’
But we have been here before with addictive drugs prescribed widely until a sever backlash over the harm they were causing. After benzodiazepines and coproxamol, could we be adding opioids to the list of shame?
How to deal with opioid abuse
Look at patient behaviour
Signs you should be looking out for include:
- Requests for extra medication
- Ordering repeat medication early
- Losing medication
- Going to different doctors in the practice
- Moving practices quite regularly
- Requests for medication that seem inappropriate for the problem
- Resistance to the idea of other modalities, such as NSAIDs or physiotherapy
- It might be worth doing an audit of your practice’s patients who are on opioids.
Check for signs of addiction or withdrawal
Symptoms such as goosebumps, dilated pupils, diarrhoea and stomach cramps may be a sign of opioid withdrawal. If you suspect the use of illicit drugs with prescribed medicines to top them up, you could do a urine screen. Where there is suspected addiction, it is best to begin an honest dialogue, which can enable you to engage the person in a therapeutic relationship.
Change prescriptions if you suspect drugs are being sold on
Patients who are selling on drugs are unlikely to admit it. You may get information from patients that they are being sold prescription drugs by other patients; this is hearsay evidence, so not something you can report to the police unless you see a potential safeguarding issue.
Document such details in the notes, but also consider restricting the prescriptions of the person involved – reduce the quantity, or arrange a review each time you prescribe.
Dr Steve Brinksman is a GPSI in Birmingham and clinical lead for the Substance Misuse Management in Group Practice network.
References
1 Prescription cost analysis, England – 2016. NHS Digital, 2016. tinyurl.com/NHSD-prescribing
2 Opioids Aware: A resource for patients and healthcare professionals to support prescribing of opioid medicines for pain. Faculty of Pain Medicine. tinyurl.com/opioids-aware
3 Chronic pain: supporting safer prescribing of analgesics,. BMA, 2017. tinyurl.com/BMA-chronicpain
4 The hidden suffering of chronic pain, Chronic Pain Policy Coalition, 2015. tinyurl.com/CPPC-hidden
5 WHO analgesic ladder: a good concept gone astray. BMJ 2016;352:i20 tinyurl.com/BMJ-ladder
6 America’s Addiction to Opioids: Heroin and Prescription Drug Abuse. National Institute on Drug Abuse, 2014. tinyurl.com/US-addiction
[Source for charts]
NHS Digital (2016) Number of painkiller prescription items dispensed in England in community from 2005 to 2015.
Please note, these figures only refer to the number of times each drug has been prescribed, and not the quantity of each prescription.

















