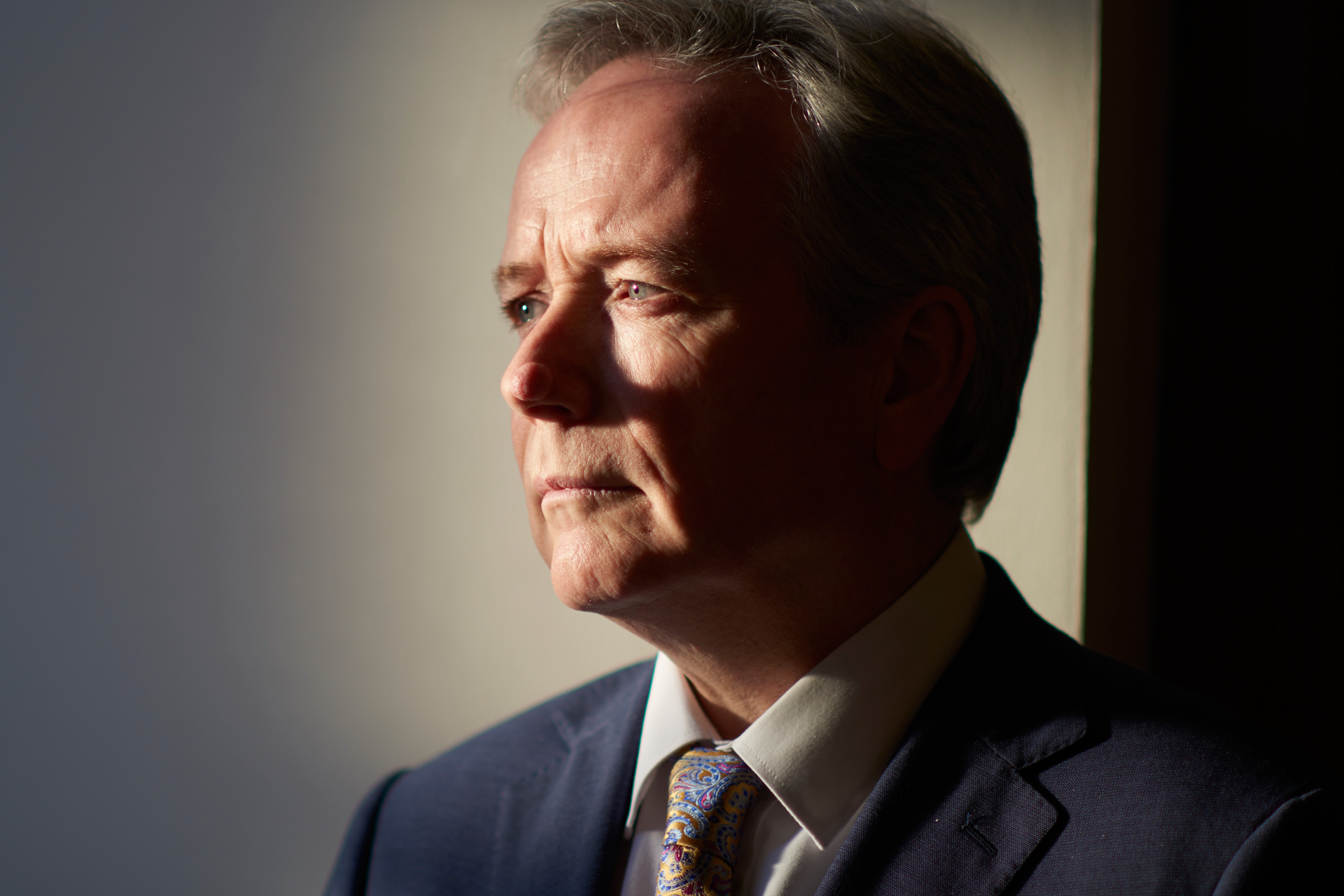
dr tom black paul stuart 3×2
Dr Tom Black, dressed in a smart suit and pastel paisley tie and full of quick-witted banter, comes across every inch the smooth negotiator.
And he needs to be, because he is spearheading one of the most radical measures ever proposed by a GP leader – asking GPs to submit mass resignations from the NHS, a move that could result in them charging patients for appointments.
The plan has the support of an overwhelming majority of the country’s GPs – around 97% – and is due to be ratified by the Northern Ireland GPC imminently.
The driver for all this is the parlous state of general practice in Northern Ireland, with practices funded even less per patient than those in England. In one town, Portadown, the profession is in danger of extinction – a situation that recently saw Dr Black apologise to a patient on live radio.
And the Northern Ireland Assembly has just collapsed, jeopardising a potential GP support package that would have seen the GPC’s action called off. Since it is the UK’s only land border with the EU, it will also be uniquely affected by Brexit. All this means Dr Black will need his wits about him as he charts a new future for general practice in the region.
Are you going ahead with the mass resignations?
There was support for the move from around 97% of all the doctors who came to the roadshows we held to gauge opinion, so I would be surprised if the Northern Ireland GPC decided to ignore that clear opinion. [Ed: The decisionby NIGPC is due later today].
You reached an agreement with health minister Michelle O’Neill before Christmas. But the Assembly has since collapsed, so is that deal now off the table?
The words of the GP rescue plan had been agreed. But there’s no timeline and there’s no investment. The next step was that the budget would be set by the Assembly and it would give its allocation to the health minister, who would then decide whether general practice was a priority or not. But now there’s no budget, no assembly. So there’s likely to be no agreement for six months, which is not acceptable.
The permanent secretary has some leverage in what he can do with the contract, but he would not have the leverage to increase the funding by 35-40%, which is what we need. So I can’t see any circumstances in which we would not start collecting practice resignations.
What did the rescue deal actually contain?
It’s very similar to the GP Forward View. It’s essentially ‘help’ in the form of pharmacists and increased GP training numbers, advanced nurse practitioners, physician associates… in other words, if you can’t get enough GPs in the next three years then you would need help from other sources. Also, it would have sent a very clear message that the Government thinks general practice is a priority.
Once the resignations had been collected, would a new Government come in to find them already in effect, or would it get a chance to honour the agreement you reached?
I think what we have at the moment is a collapse throughout general practice in Northern Ireland. Some areas are collapsing faster than others – Fermanagh and Armagh for example. Portadown is a particular problem – there is a practice with no doctors, no contractor, and none in sight. Those practices will obviously be very keen to submit resignations. Other areas such as the big cities – Derry and Belfast – have a more secure workforce, and they would be less quick to put in their practice resignations.
So, we start collecting practice resignations; we wait until we get to a critical mass – decided by the NI GPC. A problem will arise if, say, 100% of practices in one county put in resignations; do we wait until the rest of Northern Ireland is ready to catch up? I think that county would make a decision to go private – to step outside the NHS – and I think we’d have to support them with the lawyers, the accountants and even the estate agents, because some practices would be in a health centre and may not be allowed to continue in it. We have a significant defence fund of £600,000-£700,000 for that.
How much do you think people could have to pay for a GP appointment?
It’s set already by the Republic of Ireland. An appointment in Donegal, just a mile from my surgery, is €45. You go to Dublin and it’s €55. So a £45 per consultation fee is to my mind the simplest way, rather than having to set up social insurance structures with all the complications that would bring.
Some might ask how people would afford that. And the answer is, there is £240m being spent on the GP service in Northern Ireland. If we step outside the NHS, we would not make any call on that £240m. In our view, that money would be available for the Government to give to patients for fee-per-item consultations.
What does it mean for annual contract negotiations – are there any in NI?
The next step, given the hiatus in the Assembly, is that we will look for a contingency plan from the permanent secretary and the civil servants. I’ve already made suggestions to them. The way to reduce workload is to take out bureaucracy and box-ticking. So, the QOF and enhanced services should be stood down or mitigated in some way to reduce our workload.
The thing that’s really focused minds in Northern Ireland is the Portadown practice that collapsed. We tried to resuscitate it by bringing in a contractor but the contractor changed their mind about taking it on. I apologised to one of the patients on the radio yesterday, live, and said that I was sorry that we, the GPs, had failed to maintain a workforce that could provide him and his community with a service. But I think the blame for this, of course, should be served with the civil servants and the whole political arena.
All the other practices in Portadown have in excess of 2,000 patients per full-time GP. As a marker, that’s too many patients and too much work. So they’re all in a position where suddenly there are no locums and no other young GPs to over take their jobs; they’re retiring or resigning. Back in the 1950s, in my town there was one GP for every 1,380 patients. And they didn’t have all the elderly and all the chronic disease management we have. Aneurin Bevan would be turning in his grave at the current situation.
How long do you think you’d be outside the NHS before it gets settled?
Three hours. That’s how long it’d last. Patients would go to A&E because I’ve no doubt they wouldn’t want to pay for a GP appointment. It’ll be a 2,000% increase in workload for A&E. It only takes two average-sized practices to close for an A&E to double its workload. So A&E would have to bring in a charge to manage demand – higher than that in general practice – around £100.
But we have to be ready and prepared to step out permanently. There is a view in BMA House that we’re falling into a trap – that the politicians want us to go private, and they want it to be our decision and not theirs. Maybe we are. But if we stay inside the NHS with the funding levels and the workforce levels, we won’t have a GP service, so it’s not like we really have a choice here.
Do you expect Brexit to have any effect on general practice in Northern Ireland?
Yes. We’ve 1.94 million patients and 1.84 million citizens – so that’s 100,000 more patients than there are citizens. Some of those are cross-border workers, so if you live in Donegal and work in Derry, you can get a medical card in Northern Ireland and be seen free as a worker. Some of it is the natural to-and-fro across the border. I presume that
under any new dispensation, those patients might not be allowed to access the NHS. You’d think reciprocal arrangements in health will be similar to those for trade.
There’s also the issue of cross-border services; the cancer centre, radiotherapy services and paediatric cardiac surgery are all cross-border services. But I suspect that the politicians would actually just sit down and work that out. There are some EU workers, but for some reason it’s not an attractive destination for people from Europe.
Are you ballsier in Northern Ireland than the rest of the UK?
We adopt a more tribal attitude in Northern Ireland. General practice is a tribe with a common purpose and solidarity. We also have a tendency as Celts to sort out problems with confrontation rather than discussion!
CV
Age
57
Family
Married with five children
Education
1984
Graduated from University College Dublin
Career
1992-present
GP partner in Bogside, Derry
1995-2011
Western LMC secretary
2011-present
Northern Ireland GPC chair
Other interests
Gardening, and making really good raspberry jam
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens
















