Larger GP practices have lower patient satisfaction, finds report
Large-scale general practice doesn’t improve quality of care, and actually leads to deterioration in patient satisfaction, a new report has concluded.
Case studies carried out by The Nuffield Trust in collaboration with the RCGP found that larger practices did not consistently perform better on the QOF, and – in common with other practices – they continued to show a rising number of unplanned emergency admissions.
However, it also found that merging or federating to work at scale did help struggling GP practices to cope better.
It comes at a time when practices are looking to upscale, with super-practices in the East and West Midlands covering more than 100,000 patients each, while NHS England has been mandated to ensure that larger GP organisations with patient lists of more than 100,000 cover at least half of England’s population by 2020.
GP leaders said that large-scale practices have benefits for GPs themselves, but added that the report demonstrated that policymakers must ensure that they retain the local links between GPs and their patients.
The report – ‘Is Bigger Better? Lessons for large scale general practice’ – looked at two national surveys and in-depth case studies of contrasting, large-scale general practice organisations, analysing performance based on 15 quality indicators.
The authors found they were ’unable to detect marked differences in the quality of the large-scale general practice organisations compared to the national average’, with most organisations following national trends.
The report added: ’There was no consistent association between larger size and higher performance on quality measures. All three sites improved on prescribing measures and there was patchy improvement on QOF measures, but worsening performance – in line with national trends – on emergency hospital use.’
It said that upscaling allowed practices to improve efficiency through centralised management and administrative activities, maximise income and strengthen the workforce.
But it added: ’The leadership and resources needed to develop and maintain the organisation and introduce these approaches are significant.’
Especially concerning was the fact that the larger-scale operations saw a deterioration in patient satisfaction, despite offering better overall access.
The report said: ’Perhaps more surprisingly, patient satisfaction measures assessed by the national patient survey appeared to deteriorate over time, despite local efforts to improve access in each site.
’Patient interviewees highly valued their continuous, ongoing relationship with their own practice, their own doctor and the wider practice team.’
The think-tank concluded that this presented ’a difficult challenge for the leaders of large-scale general practice organisations’ as they had to figure out ’how best to harness the opportunities for efficiency and better access… but still respond to the feelings and preferences of patients who want to retain continuity of relationship and care by their usual GP’.
As part of the work, the Nuffield Trust also surveyed GP practices to find out where the development of larger-scale general practice has got to so far.
It found that almost three-quarters (73%) of practice-based respondents now work within some form of collaboration with other practices, almost half (44%) of which had formed during 2014/15.
More than half (64%) of practice-based respondents described their organisational forms as a federation of independent practices – only 2% were super-partnerships.
Dr Richard Vautrey, deputy chair of the GPC, said: ’Network arrangements should primarily be about supporting and enabling the sustainability of practices rather than trying to make radical changes to service provision that would break the direct local connection between practice and community and thereby lose the support of patients.’
Dr Maureen Baker, chair of the RCGP, said: ’This report – using data that the college has worked with the Nuffield Trust to collect and analyse – shows that large-scale general practice has a number of benefits, for both for patients and staff. In particular, it highlights how working at scale can help sustain GP services, innovate in the best interests of patients, and enable GPs to develop leadership skills.’
She added that more research was needed ’to evaluate the long-term benefits of GPs working at scale’.
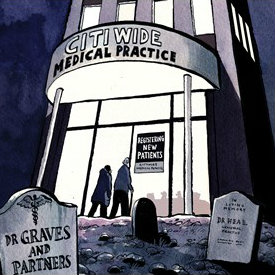
The rise of the super practice

chief inspector Steve Field – online
Source: C. Milligan
Pulse has been charting the rise of the super practice, revealing this year that one of England’s largest GP federations is contemplating a merger that could create a 540,000-patient mega-partnership.
It follows a number of other super practices, including Modality – which counts CQC chief inspector of primary care Professor Steve Field among its partners.
The GPC said in its vision for the future that super-practices could be one of the few ways of ensuring the ‘core principles’ of general practice are retained.
Lakeside Healthcare in the East Midlands told Pulse of plans to launch the largest-ever GP practice in the NHS, with 62 partners, covering over 100,000 patients.











