the great escape cover pulse final 3×2
Jeremy Hunt’s target to ‘train and retain’ 5,000 extra GPs by 2020 seems like an increasingly distant goal. Since the health secretary made this promise, GP numbers have actually fallen by 1,300.
But why? The number of GPs entering training is at its highest-ever level, almost 200 have been tempted back into the profession with the promise of bursaries and easier induction, and the NHS has started bringing in GPs from overseas. But all these efforts have been undermined by one thing – a very leaky bucket.
The Government keeps no official data on the number of GPs retiring. But for the first time, Pulse can reveal official figures from the NHS pension scheme that highlight an increasing trend towards GPs cashing in their pensions before their retirement age, causing untold damage to workforce projections.
Pulse can reveal that 721 GPs under the age of 60 drew their pensions for the first time in 2016/17 – in 2011/12 this figure was 513. Moreover, the average age of those drawing their pensions for the first time has dropped, from 60.4 years in 2011/12 to 58.5 years in 2016/17. And in some areas this is causing ‘immense pressure’ on those left behind.
There are some caveats to these figures. First, the number of GPs cashing in their pensions each year is falling, with a large decrease in the number of GPs over 60 doing so. However, this could be because so many older GPs retired when the Government first introduced changes to the NHS pensions scheme. Second, drawing pensions doesn’t necessarily mean retiring – many GPs could be taking so-called ‘24-hour retirement’, where they continue to work some sessions while drawing their pension.
But the BMA’s GP committee pensions lead Dr David Bailey believes most of those retiring early are not taking this option. ‘If you draw your pension before 60 there’s a significant [financial] hit, so I can’t see why you’d want to do that, rather than wait until you can draw it unreduced, unless you’re actually retiring,’ he says ‘A few people are coming back and doing locum work but a significant number of them are just retiring because, apart from anything else, the indemnity costs involved mean a small amount of part-time work is just no longer a feasible option.’

dr anu rao charlesmilligan 3×2
Early retirement is leaving the GP workforce on its knees Dr Anu Rao
GPs retiring report being worn down by the increasing demands of the job, scared of becoming the ‘last (wo)man standing’ or craving a life free of dastardly three-letter acronyms such as CQC or QOF. This trend is having a real impact on the stability of local health services.
Dr Anu Rao, medical officer for Leicester, Leicestershire and Rutland LMC, says the increasing number of GPs ‘fortunate enough’ to draw their pension early is leaving ‘a struggling GP workforce on its knees and creates immense pressure on GPs who are currently trying to make general practice work’. In the Yorkshire town of Bridlington, local leaders warn ‘a town without GPs is a very real possibility’, with all six practices in the town having closed their lists. Local GP leaders put this down to GPs retiring early due to unsustainable workload.
Meanwhile, practices across three towns in North Ayrshire have closed their lists to new patients for a year, with a report by the LMC pointing to the higher number of GPs retiring early. Dr Bailey pinpoints the key reason why GPs are retiring early: ‘The cause is the ongoing problem with workload and workforce that we’re seeing and we have seen for a number of years’.
Workload is reaching potentially unsafe levels. A Pulse survey last month revealed GPs have on average 40 patient contacts a day; the European Union of General Practitioners says the safe limit is around 25. The RCGP estimates GPs are seeing 60 million more patients a year than five years ago, while GP numbers have failed to keep pace.
But workload is not the only reason GPs are retiring early. The lifetime allowance for pensions tax relief was brought down from £1.25m to £1m in 2016, meaning for many GPs there is little benefit in continuing to pay into their pension fund – removing one of the main incentives to wait until retirement age.
Add in the removal of seniority payments, and the pressure of rising indemnity costs and bureaucracy, and you have a cocktail of factors with a corrosive effect on GP numbers
But it could get worse. A BMA survey of 420 GPs in 2014 found that as many as seven out of 10 were considering retiring early because of low morale or ‘unmanageable or unsustainable’ workloads, while a BBC poll of 1,000 GPs in 2015 found 55% would either ‘definitely’ or ‘probably’ leave before retirement age.
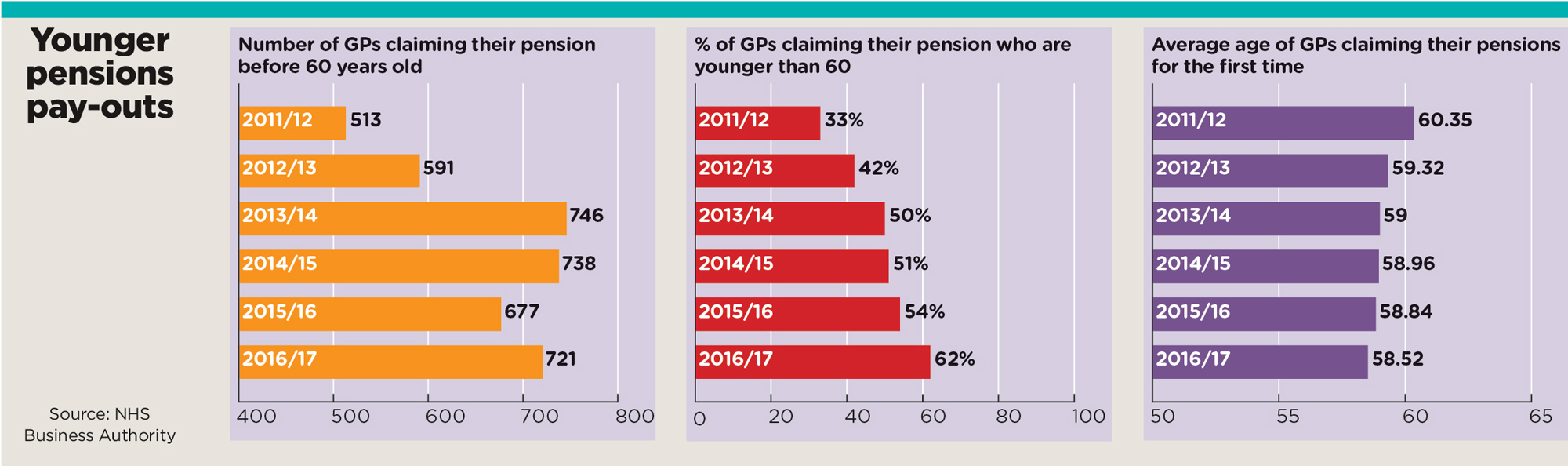
younger pensions pay outs
Why are GPs retiring early?
Workload
This is the most-cited complaint for early retirees; in a recent survey Pulse found almost half of GPs say their ability to care for patients has been affected by work stress.
Mental health
It’s a significant concern for GPs, with 500 seeking mental health treatment in the first four months of the GP Health Service.
Indemnity
According to the Centre for Policy Studies, the average GP pays £8,000 per year in indemnity costs, which is driving GPs out of the profession. Meanwhile, state-backed indemnity is not due to kick in until 2019.
Taxation
GPs with a gross income of more than £150,000 will have their £40,000 annual tax allowance on pensions contributions tapered down, with accountants advising that this will hit GPs hard in 2018.
Premises
Some GPs are retiring early to avoid a ‘last man standing’ situation, which would see them stuck with premises and staff liabilities and no one to pass it on to.
Seniority pay
Payments worth £8,000 for senior GPs were reduced by the 2014/15 contract deal by 15% a year, ahead of being abolished by 2020.
Regulation
GPC leaders have accused the CQC of subjecting practices to ‘enormous cost, workload and bureaucracy’. GPs have less confidence than other healthcare providers that the regulator is useful.6
More recently, in December 2017, an analysis by the Medical Defence Union calculated that the proportion of GPs who retire before the age of 60 had increased by 18% since 2011, which the indemnity provider linked to rising costs of clinical negligence cover. Walsall LMC medical secretary Dr Uzma Ahmad says the current levels of retirement are ‘just the tip of the iceberg’.
Dr Ahmad says: ‘Last-man-standing practices and a lack of young GP partners in some practices mean GPs are prevented from taking retirement if they want to. If these issues are resolved, then we will see even higher numbers for GPs taking retirement.’
An NHS England spokesperson said ‘fewer GPs took voluntary early retirement last year than in 2013/14 or 2014/15’, but added that ‘it is clearly going to be harder to deal with workload by increasing the number of practising GPs if, despite more GP trainees, a higher number of older GPs decide to leave their practices’.
In 2016, NHS England revamped its ‘retainer’ scheme, designed to incentivise GPs to stay on in the profession. Under the revised scheme, GPs intending to take a break from general practice will be eligible for a bursary of up to £4,000 a year if they commit to four sessions a week – 12 times higher than the previous offer. But the latest data show that, as of September 2017, the scheme has only convinced 218 GPs (90 full-time equivalents) to stay on – not yet enough to balance out those retiring.
The Government now seems to be putting its faith in importing fully trained GPs from Europe, rather than trying to keep home-grown talent in place, with a target of recruiting 600 by April and 2,000-3,000 overall, although that first target is in doubt.
The BMA is working on potential solutions. Dr Brian Balmer, a former GPC negotiator and Essex LMCs chair, says that of local GPs retiring before 60 ‘every single one, no exceptions’ has blamed workload pressures and this is the ‘key issue’ the BMA is now working on, with a new plan expected to be released next month.
Dr Balmer says this BMA initiative will be one of the first to directly address the issue of GPs retiring early, but warns: ‘We haven’t really seen anything that has had an effect on those who have decided to retire early. The retention scheme was supposed to help but it really has had minimal effect.’
He insists the key to persuading GPs against taking early retirement is to take action early: ‘Once somebody’s made their mind up to go after a significant career, trying to dissuade them I think is a waste of time.’
Additional reporting by Emma Rosser
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens