Data: How ambulance services are responding more slowly to GP calls
As part of an investigation following claims by GPs that ambulances are downgrading their calls, Pulse analysed data from the 10 ambulance services that provided figures in response to a freedom of information request on the time taken to attend patients.
All services were on average taking longer to respond when 999 calls were made by GPs or healthcare professionals, compared with those made by the general public or other callers:
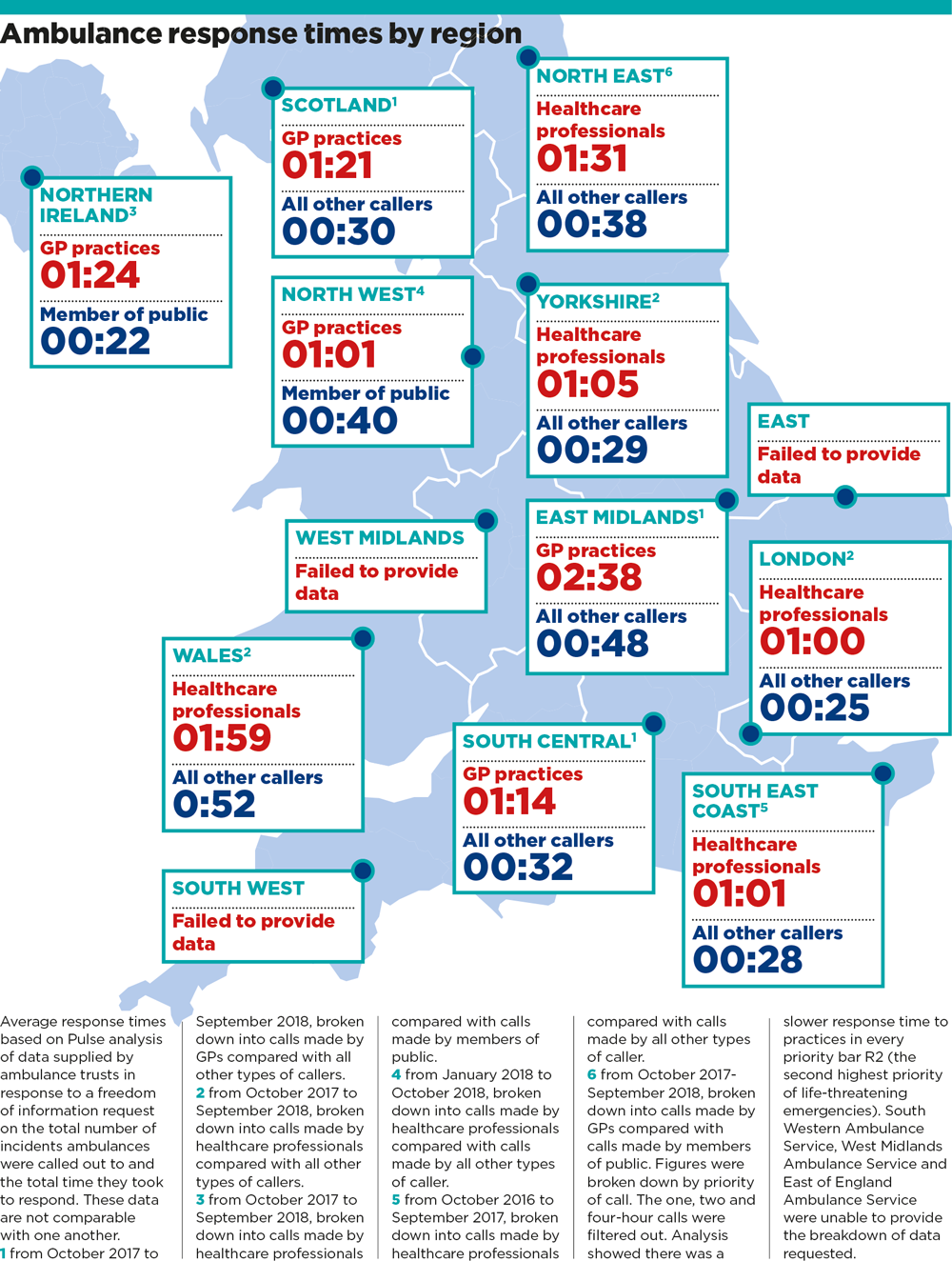
ambulance response times by region 1000x1324px
What the ambulance services say
GPs have claimed stretched ambulance services are downgrading their calls because they mistakenly believe patients are safe if a doctor and defibrillator are present – but ambulance trusts argue this is not the case.
Association of Ambulance Chief Executives
‘The Association of Ambulance Chief Executives would categorically refute any allegations that responses to patients who happen to be at GP premises or the premises of any other healthcare professional (HCP) are being deliberately downgraded by stretched ambulance services.
‘The NHS ambulance service prides itself on providing very high quality services to its patients and categorises all calls based on clinical need, in order to get to the most seriously ill patients the fastest.
‘We can confirm that there is nothing in the new [NHS England 2017] Ambulance Response Programme standards that would allow a HCP request to be treated differently to how it was in the past.
‘On the contrary, ambulance services are piloting new processes in North West Ambulance Service, West Midlands Ambulance Service (and shortly we understand London Ambulance Service and North East Ambulance Service) to improve the parity of response between public 999 and HCP requests. East Midlands Ambulance Service are also undertaking specific work in this area.
‘It is important to note that the majority of HCP requests are to schedule planned conveyance to hospital in an agreed timescale measured in hours. Very few are actually “emergency” requests.
‘The process the ambulance service is trialling is specifically designed to ensure that HCPs get parity of response for the higher acuity calls (Category 1 and Category 2). This is not to say that they didn’t in the past but in response to feedback from HCPs we are tackling it in a much more structured way with these local trials, giving us better data about performance in the future, when HCP performance will be measured separately alongside public 999 performance.’
North East Ambulance Service
Paul Liversidge, chief operating officer at North East Ambulance Service NHS Trust, says: ‘Currently, we rely on the healthcare professional who is with the patient to triage their patient and suggest a one, two or four hour response, which is not comparable to the categories within the new ambulance response programme.
‘We’re aware that some patients accessing our service via a GP may not have as good an experience as those ringing 999 for this reason.
‘Over the last year we have worked closely with our local GPs to educate them on the new categories and the information we require to be able to correctly assign the correct response to them.
‘As part of this, we have provided them with a booking checklist, combined with information about the types of skills and resources we are able to dispatch to help them when making a request. We are now monitoring the service we provide at an individual GP practice level so we can better understand any issues if they arise.
‘We are preparing to start an NHS England pilot, bringing in a new triaging process for healthcare professional requests, which should bring such requests in line with other 999 calls and ensure a consistent approach to all patients.’
North West Ambulance Service
‘We have acknowledged criticism that 999 calls from healthcare professionals have sometimes waited longer for an emergency response than we would like and in response to this, we have improved our processes and launched a dedicated number for healthcare professionals to ring for an ambulance.
‘On Monday 3 December, NWAS became one of four ambulance trusts selected by NHS England to pilot the new national healthcare professional frameworks.
‘This pilot is being undertaken in response to concerns expressed by healthcare professionals about the current system and these frameworks have been developed with their input. We also have introduced systems in our emergency operations centres to prioritise the most critical healthcare professional requests and challenge those where it appears that an emergency ambulance and/or paramedic is not the best response.
‘The trust only has a certain number of resources available across the North West at any one time and needs to effectively prioritise in order to respond appropriately. We would ask that healthcare professionals raise their concerns directly with us and we will investigate them thoroughly.’
East Midlands Ambulance Service
David Williams, deputy director of operations at East Midlands Ambulance Service NHS Trust, says: ‘We do not downgrade any 999 calls based on the qualifications of the caller, all 999 calls are categorised based on the condition of the patient. This is determined from the information provided on the initial call.
‘All calls from GP surgeries go through the same triage system as calls from members of the public. However, if the call is from a healthcare professional who has already assessed the patient, our 999 control room can work with that healthcare professional to establish what the most appropriate response is for that patient.
‘To provide a better service to healthcare professionals and patients, we launched a new urgent care transport service (UCTS) across all areas of the East Midlands in April.
‘We have already seen a positive benefit for patients with the average wait for admission reducing by half – in March 2018 the average time for a four-hour urgent transfer was 10 hours 43 minutes. Since UCTS the average wait in April reduced significantly to 4 hours 30 minutes and reduced further to four hours 10 minutes in October, work is underway to improve this further.
‘The service has been embedded as part of our operating model and the addition of further urgent care assistants means we can reach more patients allowing our frontline A&E crews to focus on our response to immediately life threatening 999 calls. Our new UCTS colleagues are an important, integral part of our accident and emergency service.’
London Ambulance Service
‘Some of the calls we receive in our control room are from healthcare professionals on a dedicated phone line. They are responsible for assessing their patient’s condition and suggesting a one, two or four hour response, when it’s not an emergency. This is not comparable to the categories within the new ambulance response programme.
‘We know that some patients do wait longer for a response than we would like, however, we have paramedics working in our control room to call patients back and assess any change in their condition. We continue to work closely with GPs locally and nationally to improve our service.’
South Central Ambulance Service
‘The data shows a difference between the mean response time for calls from GPs/out of hours (OOH) services and the mean response time from all other calls because the target response times are different, and not because GP/OOH calls are downgraded.
‘When a GP/surgery/OOH provider calls in or out of hours, the GP/HCP agrees with us what the appropriate response time is: within 1 hour,2 hours or 4 hours.
‘When a member of the public or other emergency service calls us, the calls are triaged by us as either requiring a response within under seven minutes (average, category 1), under 18 minutes (average category 2), within two hours (90th percentile, category 3) or within three hours (90th percentile, category 4).
‘Nearly 60% of our member of the public/other calls are triaged as category 1 or 2 responses (average response expected within seven or 18 minutes), and only 3% are category 4 (90% response within three hours) so given that there is a much higher volume of 999 calls that we respond to from members of the public/others that require a quicker response than calls received from GPs/OOH providers, it would be completely normal for the average time of all the GP/OOH providers to be longer.
‘In terms of our process, when calls from GPs or other HCPs are not responded to within the one, two or four-hour limit, then our clinical support desk will call them back to see if the patient’s symptoms require re-triaging.’
South East Coast Ambulance Service
‘All our 999 calls are triaged in the same way and assigned an appropriate response based on information provided by the caller. We work hard to prioritise our response to our most seriously ill and injured patients.
‘It should be noted that the figures for HCP calls will also include our response times to calls where an HCP has specifically requested an ambulance attendance within a particular time ranging from one to four hours.
Northern Ireland Ambulance Service
‘The Northern Ireland Ambulance Service would not agree with any suggestion that we downgrade GP calls.
‘All emergency calls received in our emergency ambulance control centre are triaged through an internationally recognised medical priority despatch system which categorises calls based on clinical need only.
‘NIAS would respectfully advise that the information provided under FOI includes “card 35” healthcare professional (HCP) category calls, which although included in category C emergency calls, reflect those calls where timeframes (of up to four hours) for response have been agreed with the GP. This will explain the disparity which has been identified in average response times. A more accurate comparison would have been calls not including HCP calls.’
Scottish Ambulance Service
‘GPs request emergency and non-emergency ambulance responses. We have undertaken significant engagement with the GP community to ensure they are fully informed when booking ambulance resources.
‘When an emergency response is requested it is given the same priority as a 999 call from the public. We are continuing to work with the GP community on further improving this process. The Scottish Ambulance Service does not downgrade requests for ambulances made by GPs or healthcare professionals.’
Welsh Ambulance Service / Yorkshire Ambulance Service
Declined to comment









