A new contract is born, but is it Scottish GPs’ saviour?
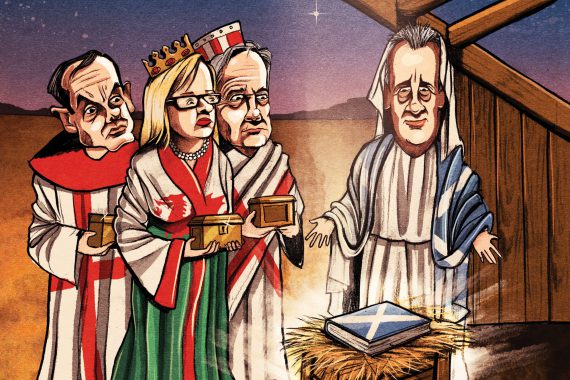

3wisedoctors illio©ben jennings 3×2
General practice in Scotland is set for its biggest overhaul since the 2004 contract.
A new deal has been agreed between the BMA and the Scottish Government that aims to transform the day-to-day function of the GP.
Gone will be the crippling risk of running a practice and the tedious box-ticking to chase small pots of funding, with GPs able to focus on being clinicians again – or so the theory goes.
As Dr Alan McDevitt, chair of the BMA’s Scottish GP Committee, puts it: ‘We talk about having GPs being GPs. You don’t have to be an entrepreneur to work in general practice. We want GPs to be clinicians most of the time.’
GPs’ role will become that of ‘expert medical generalist’, providing clinical leadership to a primary care team of pharmacists, physiotherapists and paramedics among others, who will share the clinical workload, taking on work that does not need a GP’s expertise.
The plan is that GPs will then have time to focus on complex cases and will be in a position to provide these patients with genuine continuity of care and offer longer consultations where needed.
However, the lofty ambitions set out in the deal may not be easy to achieve, with some GPs warning the measures won’t be enough to free up the time needed.
For others, the concerns are more ideological. Critics see the contract as representing a part-nationalisation of general practice, with the state intruding on a model that has worked well for years and simply needs better funding.
GPs tell us they want less bureaucracy – we have achieved that – Shona Robison
They say this will remove much of the potential for entrepreneurialism that has been the hallmark of general practice for so long, and will leave the profession at the mercy of the state. Even Dr Miles Mack, who stepped down as RCGP Scotland chair last month, has expressed concern.
‘The autonomy GPs have will be lost, with no assurance on workload control and T&Cs far short of those of consultants,’ he says.
For proponents, the so-called ‘Scottish Blue Book’ is a radical solution for a profession in crisis. Practices are already effectively being nationalised as they fail and are taken over by the NHS through health board management, and growing numbers are closing their lists to new patients – 40% of those in Edinburgh for a start. Everyone agrees something has to change.
Funding concerns will be addressed: there will be a £23m injection next year, which the GPC estimates will mean a boost for two-thirds of practices.
Furthermore, from April 2019, no full-time GP partner will earn less than £80,000 a year, inclusive of pension contributions, with one in five GP partners benefiting as a result. ‘It’s unacceptable that full-time partners earn less than £70,000 a year,’ Dr McDevitt says.
WHAT’S IN
- No practice will lose funding under the deal; two-thirds are expected to see a funding boost next year, with £23m invested in a new formula that prioritises practices with elderly or deprived populations.
- No GP will earn less than £80,430, from 2019.
- In 2020, GPs will see their pay move on a par with that of consultants and direct reimbursement of practice expenses – subject to a second poll of the profession.
- In smaller, remote GP practices, ‘extra resources will continue to be made available to ensure long-term sustainability’ and that they can provide the broad range of services needed in a remote setting.
- From April 2018, GPs will have one extra session per month of protected time for ‘clinical leadership’, extending to regular protected time for every GP.
WHAT’S OUT
- There will be a gradual nationalisation of GP premises, with the intention that no GP will own theirs by 2043. GP partners will be given five-yearly loans, interest-free, to support premises liabilities up to that year.
- GPs will no longer be responsible for tasks such as prescriptions, acute and minor illness, and chronic disease management – these will be transferred to other members of a GP-led multidisciplinary team.
- Responsibility for immunisations will move to health boards, while maternity and contraception services will continue to be provided by community teams.
- A community team will manage minor injuries and chronic disease monitoring, as well as dressings, phlebotomy, ear syringing and suture removal.
- Physiotherapists will provide treatment for musculoskeletal presentations, community mental health workers will provide care and link workers will signpost patients to non-clinical services.
- Scotland ditched the QOF a few years ago – this will be replaced by a system of GP quality improvement in clusters.
And what we still don’t know…
- Whether GPs will vote in favour of the contract. A special LMCs conference at the start of this month will be followed by a ballot of the profession.
- What the pay ranges will be for GPs, and how their personal income will be defined GPC and Government to decide after a data-collection exercise.
- How staff expenses will be calculated GPC and Government to decide after a data-collection exercise.
- How precisely GPs will be freed up for the role of ‘expert medical generalist’, offering longer appointments Local areas to come up with plans on how to redesign services.
But the longer-term strategy is more radical. The agreement is moving towards set pay for GPs ‘comparable to consultants’. Under the new system – which will be introduced for 2020 subject to a ballot of the profession – there will be ‘pay ranges’ for GP partners, with a new system of pay progression.
This has huge ramifications. It will, in effect, see GP drawings determined, and guaranteed, by the NHS.
In a similar vein, the NHS is set to take responsibility for employing more members of the multidisciplinary teams, including pharmacists, physiotherapists, mental health professionals and link workers, attached to practices or clusters. As well as this, it will take on the responsibility for vaccinations and urgent care services, such as emergency home visits.
GPs will focus on three key areas: patients presenting with undifferentiated conditions, continuity of care for patients with complex conditions and clinical leadership of the team.

shona robison 330x330px
Scottish health minister Shona Robison says: ‘GPs tell us they want to spend more time with patients with undiagnosed illness and less time on bureaucracy, while patients say they want better access. We have listened and, I believe, we have achieved that balance.’
How this will be done in practice is still up for discussion. Health boards have been instructed to work with GPs to redesign the system, and will also be responsible for monitoring GP workload.
The NHS will also indirectly have more say over practice staff, as it will be directly paying their expenses from 2020 – with the global sum reduced accordingly. Again, how this will work in practice has yet to be determined but the fear is that a ceiling will be set on staffing costs for each practice.
All this is quite different to the approach taken in England, where groups of practices are being tasked with taking on more staff, more services and more risk, under plans to shift care out of hospitals set out in 2014 by the Five Year Forward View.
One of the central aims of the new Scottish GP contract is to make partnership more attractive for younger GPs, to help tackle the huge recruitment problems that have left one in four practices with at least one GP vacancy, almost three-quarters of which have been open for six months.
One key way it tackles this is by diluting the risk of ‘last man standing’, whereby the final partner to retire or resign is left with the full burden of premises liabilities. Practices will be offered loans to help cover the costs of premises, with the intention that GPs will ‘no longer own their premises’ by 2043.
And Dr McDevitt rejects the idea this agreement represents the end of the independent contractor status. He tells Pulse: ‘People get very hung up, as if it is a binary choice; the independent contractor model was much more about being free of management.
‘GPs will still employ the same staff they have now, the money comes into the practice and the partners decide how to spend it, so these parts of independent contractor status are just the same. What we are doing is reducing the risks. We’re not planning to be employed and the Government doesn’t want us to be.’
But there is a risk others don’t see it that way. For instance, Pulse has learned of concerns that HMRC could look at the deal and decide to tax GPs as employees of the Scottish Government. Dr McDevitt says the GPC is ‘alive to this issue’ and is taking advice at every stage to ensure this does not happen.
There may also be a problem with rural GPs, for whom a multidisciplinary team approach may be less applicable. The Scottish Government has promised them extra resources to ‘ensure long-term sustainability’, but rural GP leaders say it has ‘fallen short’
In any case, the deal is not yet set in stone. The start of this month sees a special LMCs Conference in Glasgow, where local leaders will meet to vote on the contract. If they vote in favour, there will be a ballot of all GPs in Scotland.
A Pulse straw poll of more than 200 GPs in Scotland shows the majority are ‘undecided’ on the deal, although the BMA has started a series of roadshows to convince grassroots GPs of its merits ahead of the ballot.
If GPs vote against the new contract, the status quo will remain. But if, as expected, the new deal goes through, there will for the first time be clear blue-and-white water between the Scottish model of general practice and that in the rest of the UK.
A disunited kingdom?

england flag 330x330px
As Scotland plans its part-nationalisation of general practice, England is heading in the opposite direction. NHS England’s Five Year Forward View is more concerned with encouraging GPs to merge in federations to provide more services to populations of at least 30,000 patients.In some areas they are busy building even bigger structures. Manchester, where health is fully devolved, is planning to form ‘accountable care organisations’ that will put all primary, secondary and social care in the same funding pot, with the GP federation sitting on a governance board including local government and CCGs.While the destination looks similar to Scotland’s – for instance, Manchester recently published plans for practices to hire paramedics for home visits and to offer half-hour appointments – the route map is very different.

northern ireland flag 330x330px
In Northern Ireland, the direction of general practice contrasts even more starkly with Scotland. The NI GPC is currently collecting resignation letters from practices as part of a plan to remove them from the NHS altogether and begin charging patients for services. Chair Dr Tom Black supports the Scotland deal, but says GPs in Northern Ireland are ‘more wedded to the independent contractor model until we see where things are politically’.
welsh flag 330x330px
Wales has always had a model much closer to Scotland’s, and may even copy the deal reached there in future. For instance, assistant medical director at NHS Wales and GP Dr Sally Lewis said on Twitter: ‘The proposed new Scottish GP contract is inspired, bold and exactly the way we should be heading in my opinion.’ Watch this space
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens










