It is starting to become clear that the implications of the national review of PMS funding are potentially devastating for the practices involved.
Three months into the two-year process of reviewing all PMS contracts, practice accountants are saying their clients are preparing to lose up to £400k per year and they are advising them to cut back on staff and reduce patient services to avoid going under.
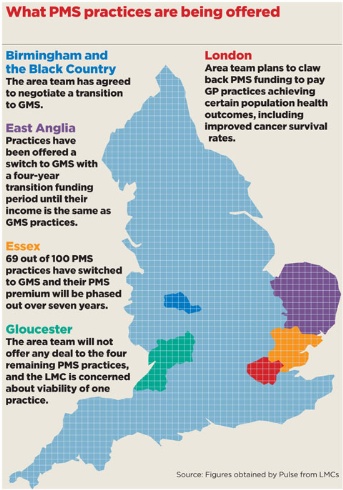
LMCs across the country are trying to negotiate parachute payments to mitigate the losses, but their efforts have met with a mixed response. While some area teams are happy to fund measures to ensure the viability of practices in the short term, others are blocking such plans.
Meanwhile in London, managers are planning for practices that remain on PMS contracts to be paid based on outcomes, including increasing cancer survival rates.
Equal opportunities
In February, managers announced a two-year review of all PMS contracts, after a fact-finding exercise showed £260m of so-called ‘PMS premium’ funding above that given to GMS was not linked to additional services. This review is ongoing, led by local area teams, aimed at ensuring ‘equality of opportunity’ for GP practices, with the possibility that funding could be shared out across primary care.
The announcement came amid declining numbers of PMS practices, with the 3,270 in 2012 representing a decrease of 45 on 2011.
But it is only now that the impact on practices is being understood, with accountants issuing ominous warnings.
Essex accountancy firm Edmund Carr has warned the practices it is advising they could face total reductions ranging from £50k to £400k, because this funding is not linked with specific services, although it says cuts towards the top end of that range will be exceptional.
But the firm is not the only one warning of six-figure annual losses.
Bob Senior, chair of the Association of Independent Specialist Medical Accountants and Baker Tilly’s head of medical services, says: ‘You are probably looking at [potential losses of] between £50,000 and £150,000 for a typical PMS practice, with three partners.’
Losses on such a scale would leave some practices unviable unless they make drastic changes, he says.
‘If you are being funded as if you were GMS, then you need to change your services back to match GMS. If you do nothing with the staff… then you’re probably going to be financially unviable.’
In order to mitigate these losses, many local LMC leaders have already begun negotiating deals to give practices transition payments if they switch to GMS contracts now.
In Essex, PMS practices will have their ‘premiums’ – the money they receive that is not linked to providing services above GMS – phased out over seven years.
The deal has been taken up by 69 out of 100 PMS practices in the county, and has been welcomed by GP leaders and accountants, who view this as the most sustainable option for PMS practices.
Essex LMC chair Dr Brian Balmer says: ‘The alternative is extremely uncertain and could be a cliff edge of financial reduction, a very sudden chop of financial resources.’
East Anglia has followed Essex’s example, but with a four- rather than seven-year transition, which local accountants warn may not be adequate.
A similar situation, also setting off alarm bells, has developed in West Yorkshire, where the LMC says practices are being offered only ‘a couple of years’ of transition payments if they switch to GMS.
In Birmingham and the Black Country, Berkshire, Buckinghamshire and Oxfordshire, Leicester and Rutland and Lincolnshire, LMC leaders are hoping to be able to reach the same deal as in Essex, with a full seven-year phase-out before receiving GMS-level payments.
But in some areas, practices are being offered no help at all. In Gloucester, where only four PMS practices remain, the area team has refused any deal, saying a similar deal was struck with the PCT two years ago.
Badly hit
In other areas, GP leaders fear the worst. In Wakefield, West Yorkshire, the local area team is aiming to reduce the funding given to PMS practices from £90 per patient to £78 over the next four years.
Wakefield LMC chair, Dr Andrew Sykes, says that as the town is ‘the second biggest PMS area in West Yorkshire, and West Yorkshire is an outlier in England’, this will badly hit Wakefield in particular.
‘We’re looking at losing about 19% of our [primary care] spend in terms of money going out. That equates to 20 whole-time-equivalent GPs.’
For practices that decide to stick with PMS, there is also another potentially dark cloud on the horizon.
In London, plans to a pilot a new one-size-fits-all contract for PMS practices will make any additional funding above GMS dependent on how well they achieve certain population health outcomes, such as increasing cancer survival rates.
The NHS England London area team says the plan is aimed at helping to ‘reduce health inequalities’.
Across England as a whole, managers are stressing fairness. An NHS England spokesperson said: ‘We have put in place a clear framework to ensure extra investment in PMS is fairly and transparently linked to quality of care for patients or the particular needs of the local population.’
The GPC is critical of the inconsistent approach across area teams. Chair Dr Chaand Nagpaul says: ‘It appears illogical that although NHS England is a single organisation, individual areas are taking such divergent approaches.
‘When areas are agreeing on a return to GMS on terms that are acceptable, it makes no logical sense to create barriers in other areas. I think this is something we will be taking up nationally.’
Benefits for GMS practices
But while GP leaders and accountants are concerned for PMS practices, those on a GMS contract may welcome moves to give them access to this additional funding.
Dr Nagpaul says: ‘It is absolutely crucial that every pound of the PMS resource is invested back into general practice. We hope both PMS and GMS practices will be able to earn that money back by taking on enhanced services.’
However, he concedes: ‘We need absolute certainty and evidence that it is being reinvested [and] there is nothing currently that forces them to do that.’
But NHS England’s head of primary care commissioning Dr David Geddes, a GP in York, says this is one of the aims of the review.
He says: ‘Whether a GMS or PMS practice, you should still have access to innovating funding so we can work with you to identify ways of developing, operating, primary care at scale.’
But for Dr Nagpaul – a PMS partner in London himself – the future of PMS is not looking bright. He says: ‘I hope I get out of PMS by then. We are just doing the sums, with all the other contract changes, to see the feasibility [of switching to GMS].’
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













