Ghost patient drive comes back to haunt GPs


GP practices are at the centre of an unprecedented drive to remove so-called ‘ghost’ patients from their lists.
The rolling three-year programme is projected to save the NHS £85m, but a Pulse investigation reveals it has removed thousands of genuine patients, blocking them from accessing health services.
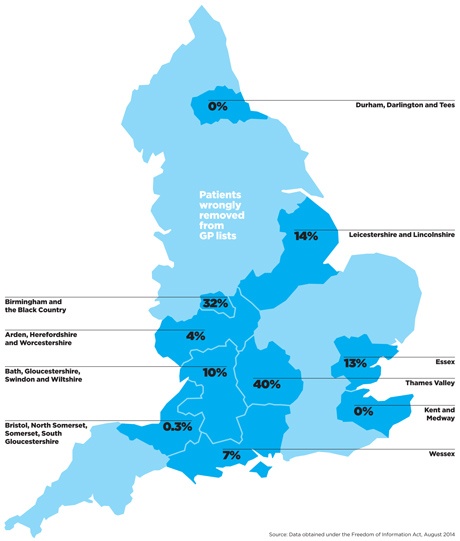
Of the 4.8 million patients who have been reviewed already, 4.2% have been deleted from lists, but in some areas up to 40% of these patients were genuine and have had to re-register with their practice after discovering they had been removed.
NHS England says it takes ‘all possible steps’ to contact patients before removing them from GP lists, but GPs say they are targeting vulnerable groups, causing great distress for patients and causing some to miss key appointments as a result.
In one case, Pulse has learnt that students were removed from a GP’s list without first being contacted, after area team managers simply asked the local university whether they still resided there.
The programme began last summer, with NHS England publishing a national policy to target the very elderly, children and those in multiple occupancy homes to ensure that ‘list inflation is appropriately managed’.
NHS England’s guidance says area teams are expected to engage in ‘regular proactive list management with general practices’ to ensure that practices are being paid for genuine patients and that those with 5% more registered patients than head of population ‘will be benchmarked against their achievement in reducing lists’.
Three-year plan
Area teams have been instructed to validate all GP lists continuously over a one to three-year period, and they are making remarkable progress. Data obtained by Pulse under the Freedom of Information Act shows that 20 of the 25 area teams have begun work to validate GP lists since last year. Of the 10 able to provide figures, they have removed some 200,000 patients from lists so far.
But 14% of patients have subsequently re-registered with their GP, an error rate double that for previous PCT schemes – a Pulse investigation last year found 7% of patients under list-cleansing schemes had to re-register with their GP in 2012/13.
The Thames Valley area team had the worst rates, with re-register rates of more than 40% for its scheme, 32% for the Birmingham area team and 14% in Leicester and Lincolnshire. Extrapolated across the whole of England, this would mean around 35,000 patients eventually being wrongly removed from GP lists under this programme.
For GP practices in affected areas this is a huge problem. These reviews are leading to severe distress when patients find out they have been removed from their practice’s list – and GPs inevitably take the blame.
Dr Sally Whale, a GP in Ipswich, says: ‘We probably have several every month who find they have been removed from our list without their knowledge.
‘They are usually confused and angry, as being told you aren’t registered when you need an appointment causes worry,’ she says.
Dr Louise Irvine, a GP in Lewisham, south east London, says that ‘loads and loads’ of patients have been wrongly removed from her patient list. She adds: ‘Patients were very distressed at being removed.
‘We try to re-register them as quickly as possible to stop this interfering with their care or their ability to get an appointment, but it leads to a lot of time being spent by our receptionists who are already very busy, trying to explain what happened and getting them to fill in the registration forms again.’
What GPs are saying
Sometimes there are angry scenes at reception, which is distressing for everyone.
Dr Louise Irvine, Lewisham, south-east London
The distress to the patient is the most significant part of this intervention.
Dr Rachael Kenyon, Clevedon, Somerset
We already ‘clean’ our lists regularly – we check for non-responders for QOF, flu and other targets.
Dr Richard Ma, Islington, north London
The majority of patients removed recently seem to be women who have not had a smear test in the last five years.
Anonymous GP
Patients are often abusive when told they need to register first then get an appointment.
Dr Peter Goodall, Southampton.
Angry patients
This tension can spill over into the practice itself, she adds: ‘We tend to get the blame. People don’t realise that it’s the health authority, not the practice that is doing this. Sometimes there are angry scenes at reception, which is a distressing situation for everyone.’
NHS England has told area teams to choose particular ‘cohorts’ to focus attention on. They include patients over the age of 100, addresses ‘with apparent multiple occupancy’ and patients who have missed an NHS appointment – for instance, for childhood or flu immunisations, or cytology.
But this approach is leading to some patients missing vital appointments and compromising care, say GPs.
Dr Tony Grewal, medical director of Londonwide LMCs – an area where 116,479 patients have been removed in a massive list-cleansing drive by the area team since last September – explains: ‘It is rare that a letter sent to somebody living in a multi-occupancy residency will get to the right person.
‘Very often these people don’t speak English as a first language, or don’t understand the importance of a letter they get from NHS England. Those seem to be the higher proportion of the removals. But they are also more likely to be a vulnerable group and it has been a concern for us.’
Dr Sanjeev Juneja, a GP in Rochester, Kent, said a three-year-old child on his list had been targeted by his area team because he failed to return a letter. ‘Vaccinations were missed as the child was not listed,’ he says.
Another GP, who wishes to remain anonymous, says that he found out a single mum with several children had been removed from his list after they were flagged as living in a house with ‘too many other people’.
He adds: ‘Unfortunately all of them had been under child protection at some point or other. My concern is that they could have been in a situation where the children could have been harmed, with no GP to pick that up.’
Related articles
‘We’ve had patients here for years who have suddenly been removed’
Overzealous ghost-hunting is damaging patient care – it must stop
Burden of proof
As well as the effects on patient care, the programme is causing practices piles of administration to prove that patients are genuine.
NHS England sends two letters to suspected ‘ghost patients’ and if there is no response then a FP69 flag is put on the patient’s record in the GP’s computer system. A database of these flags is then sent to practices, which are given six months to check whether they are valid or not before the patient is removed from their list for good.
But for many practices, this is a huge amount of additional work. One practice manager in a university city, who did not wish to be named, says it is a particularly big issue for him, as students are a big focus of the list validation exercises.
He says the local area team wrote to the university to find out whether students were still living there. It used the say-so of the university offices to determine whether the students should be on the patient list or not.
He adds: ‘The last database I was sent had 1,700 names on it. They have not written to each of these people, they have acted on the hearsay of an administrator. They give us six months to tell them otherwise. We cannot afford to lose 1,700 patients.’
Because most of the students live off the university campus, the practice manager retained ‘around 80% to 90% of the patients on the database’ – but only after a huge administrative exercise. ‘It is completely a crude way of doing this,’ he adds.
Dr Jacqueline Marshall, a GP in Uxbridge, Middlesex, took drastic action to prevent her patients suffering. She says: ‘I’ve had to spend weekends in the practice obtaining evidence to prevent patients being removed erroneously. The list included the most vulnerable, for example older people, people with dementia, and mental health patients who did not reply to letters.’
It’s not the first time there have been list cleansing drives. Pulse reported last year that PCTs were undertaking last-minute efforts to review their practice lists before handing over to NHS England, after the DH instigated a list-cleansing campaign in late 2011 to remove up to 2.5 million ‘ghost patients’ from GP lists across England.
But now, with NHS England facing extreme budget constraints, managers are facing even more pressure to trim their primary care budgets, and this scheme is an attractive way of reducing GP spend as it means they can cut £73 in annual global sum payments for each patient removed.
Savings
The first paragraph of NHS England’s policy states that ‘if a patient list is overstated, the contractor will receive more funding than it would ordinarily be entitled to and this presents a significant financial burden on NHS resources.’
It quotes 2010 figures from the Office for National Statistics (ONS), which estimated that the number of people on practice lists exceeds the national population by ‘approximately 2.8m people, which is equivalent to 5.2% inflation’. As a result, reducing the average percentage to 3% ‘would realise indicative savings of around £85m’.
And this money will be recouped directly from practice income. For a practice that has 200 patients taken off the list, this equates to a £15,000 reduction in income per year. Even wrongly removed patients that are later put back on patient lists could still have an impact on practice income as payments are based on the list size as recorded on a particular date.
NHS England says it is doing all it can to prevent distress to patients. An NHS spokesperson says: ‘NHS England takes all possible steps to contact patients and minimise the number who need to re-register – but there will always be some circumstances where patients do not respond and at that point we have to assume they have moved away and are therefore not in reality receiving services from that GP.’
Managers also took issue with the assumption that all patients who were removed and had to re-register were ‘wrongly removed’. The spokesperson added: ‘Patients can always re-register with that practice or another. It is therefore incorrect to say that they have been “wrongly removed”.’
But Dr Robert Morley, chair of the GPC’s contract and regulations subcommittee, says Pulse’s figures show the policy is ‘lunacy’ and that managers should be concentrating on other things, rather than chasing phantom cost-savings from general practice.
He says: ‘There will inevitably be swings and roundabouts, balancing “ghost” patients with unregistered patients.[But] to claim general practice is unfairly overfunded by the existence of ghosts is a complete fallacy.’
NHS England’s plans to validate GP lists
NHS England has issued a framework to local area teams of operating principles for list-cleansing drives. It says:
• Area teams must work through practice registers as a continuous rolling programme of checks over a one- to three-year period.
• This could include phased targeting of specific patient cohorts, including those who are part of screening programmes, patients aged 100 years or older, addresses with multiple occupancy, and university students.
• Practices should screen proposed cohorts in advance of any letter-writing exercise.
• Routine letters sent by practices that are returned by Royal Mail result in practices being given six months to provide confirmation of the patient’s address.
• NHS England says ‘where confirmation… cannot be provided the patient is removed from the practice’.
Source: NHS England: Tackling list inflation for primary medical services, June 2013
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













