Special report: The NHS reforms one year on
Who is leading commissioning?
A Pulse investigation last September found the proportion of GPs sitting on boards had fallen to 43%; a similar investigation in 2012 found GPs occupied 49% of the positions on boards.
More recent data seen by Pulse and compiled by False Economy – a campaign group funded by the TUC – backs up these figures and shows GPs are now in the majority on fewer than a third of boards.
In South Tyneside, for example, just two board members out of 12 are GPs. However, Dr Matthew Walmsley, chair of NHS South Tyneside CCG, tells Pulse: ‘The GPs in our organisation are in positions where they can lead major change in South Tyneside. We built our constitution carefully to enable them to do that from outside our governing body. I believe that, for a small CCG, our financial stability and increasing national recognition as innovators are indicators of the success of that approach.’
Do GPs feel involved in commissioning?
A Pulse survey reveals that grassroots GPs feel even less involved in commissioning a year after CCGs took control.
The proportion who said they feel more involved in commissioning under CCGs than under PCTs has fallen to 33% from 36%. The proportion of those who do not feel involved in commissioning increased by eight percentage points to 63%.
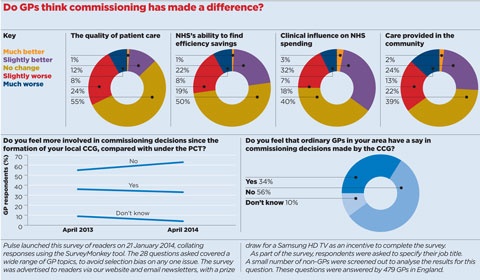
Of 479 GPs who answered the survey this year, the majority – 56% – said they felt ordinary GPs had no say in commissioning decisions made by the CCG.
A majority of GPs also felt the switch to CCGs had not improved the quality of patient care or the NHS’s ability to find efficiency savings.

The LMC leader: ‘GPs now have conflicting priorities’
It was inevitably going to fail. CCGs are going to end up like any other commissioning organisation – they are statutory bodies with statutory functions, the most important of which is to stay within budget.
[Membership of the CCG] will have to come into GPs’ decision making, even subconsciously. They will want to do what is best for their patients, but practices are now part of CCGs.
But there might also be concerns from patients that GPs are making decisions that are not in their best interests. I don’t believe any GP is doing that consciously, but they have been put in a situation where they may have conflicting priorities.
Dr Robert Morley, secretary of Birmingham LMC
But there are two areas in which a significant number of GPs feel CCGs have made more of an impact.
Some 35% of GPs said the move from PCTs had meant greater clinical influence on NHS spending, while 26% said the amount of care provided in the community was better under CCGs.
Dr Robert Morley, secretary of Birmingham LMC, says: ‘Most GPs have a CCG that tries to engage and a constitution that is fit for purpose, but they still feel that decisions are made by the leadership of CCGs, heavily influenced by NHS England and commissioning support units, and that there is only lip-service paid to the involvement of grassroots GPs.’
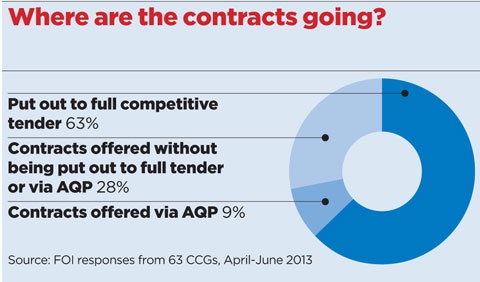
How have CCGs used competition?
The use of competition by CCGs has been muted in the first year.
Some large, high-profile contracts have seen interest from private companies. Cambridgeshire and Peterborough CCG is running a procurement process for a contract worth £800m to provide elderly care. Chief clinical officer Dr Neil Modha stresses the care ‘will remain NHS-funded, provided under an NHS contract and free at the point of delivery’, although the private sector was heavily represented among the final four bidders – Accord Health, Care for Life (including Care UK), Virgin Care, and the hospital-led provider organisation, Uniting Care Partnership.
Early on, several major contracts for community services were signed with private companies. In 2012 Virgin Care won a £500m contract in Surrey, while Serco was awarded a £140m deal in Suffolk.
An investigation by Pulse last year based on FOI data from 63 CCGs found in the first three months since April 2013, 63% of the new contracts offered by CCGs were put out to full competitive tender and 9% out to Any Qualified Provider.
Essex LMCs chief executive Dr Brian Balmer says: ‘We are galloping towards privatisation. The procurement rules are quite destabilising to the whole system. They have introduced the ethics of the marketplace to a crucial public need.’
In some cases, though, commissioners have awarded contracts to GP practices without inviting competition. NHS Rotherham CCG recently extended its existing GP-held contracts, saying only practices could ensure the ‘safety, quality and accessibility of these services’. Brent Council also allowed GPs to retain all public health enhanced services.
Related articles
Dr Michael Dixon: ‘For heaven’s sakes, let CCGs lead’
But these may become the exceptions. Under Section 75 of the Health and Social Care Act, all services must go out to tender unless it can be proved they can only be delivered by one provider.
The situation with Blackpool CCG and Fylde and Wyre CCG highlights the potential risks for commissioners. Monitor, the healthcare regulator, is currently investigating a complaint from Spire Healthcare Limited claiming that the CCGs asked GPs to direct patients away from Spire Fylde Coast Hospital and towards Blackpool Victoria Hospital. The CCGs deny the allegations.
Dr Steve Kell, co-chair of NHS Clinical Commissioners and chair of Bassetlaw CCG, says: ‘None of us go into clinical commissioning to privatise the NHS.
‘Where there are gaps in services, I have no doubt we will commission from the private sector. But it is not about privatising the NHS – it is about improving local services.’

A year since the official launch of the CCGs, GP commissioning has made no difference
Retired locality chair Dr Peter Rudge argues that the only way to change the system now is to involve patients
Are CCGs managing to balance the books?
Board papers from NHS England have revealed that, at the end of January, 24 CCGs were forecasting a deficit by the end of the financial year – almost three times as many as the nine that had forecast a deficit in April 2013.
Even so, GP commissioning leaders have claimed this is a good result at a time when the health service is experiencing its toughest financial climate for years.
In his Big Interview published last week, Dr Michael Dixon, interim president of NHS Commissioners, says: ‘They have run it better than the previous lot, because they are running it in a financial deficit situation and most of them are making ends meet. That is credit to the frontline GPs, who are looking at their prescriptions, use of diagnostics and the rest. They are fully joined into the system in a way they never were since 1 April last year.’
Nevertheless, Dr Dixon warns CCGs are being used as the ‘risk pool’ of the NHS, with several surprise bills for PCT legacy debts and the top-slicing of budgets to fund specialist services challenging even the most financially prudent CCGs.
Dr Dixon says: ‘How on earth can you plan budgets when you are being eternally told you have to pay debts that you never accrued yourself, or which are for overspends in secondary care over which you have absolutely no say?’
There is also controversy surrounding the disparity in the funding allocations given to CCGs for the next two financial years.
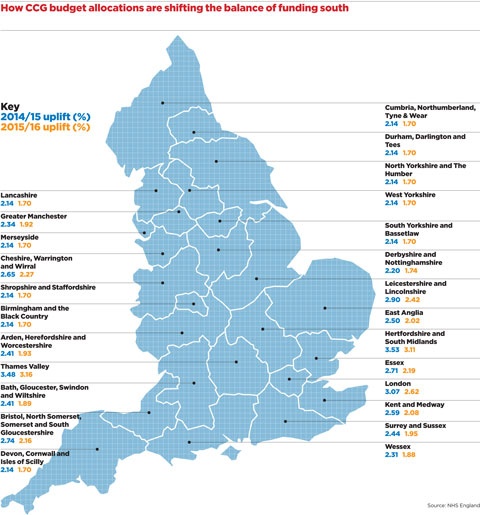
Funding increases are much higher in the south, with only nine out of 78 CCGs in the north of England awarded more than the minimum uplift of 2.14% and 1.7% for 2014/15 and 2015/16 respectively. That is in stark contrast to the Thames Valley area, for example, where nine of the 10 CCGs have been awarded at least 3.3% and 2.8% for the two years respectively. Experts from Durham University have claimed this will worsen the north-south divide and ‘reduce NHS services in the north’.
What areas are CCGs prioritising?
GP commissioners are prioritising reductions in emergency admissions and increases in dementia diagnosis rates, figures revealed by Pulse last year show.
CCGs were asked to select a number of local targets for achieving the quality premium, in agreement with local area teams and health and wellbeing boards.
A target of reducing emergency admissions within 30 days of discharge was selected by 29 of England’s 212 CCGs in 2013/14 and boosting diagnosis rates for people with dementia was chosen by 27.
Other popular indicators include improving functional ability in long-term conditions, the proportion of people with diabetes who have received their nine annual care processes and enabling people to choose their place of death.
The local choices are separate from the centrally mandated targets set by NHS England. Together, they are worth up to £5 per patient for CCGs, although a Pulse survey of 39 CCGs last month found none expected to receive their quality premium payments in full.
Clinical commissioners do seem less eager to spend money on management consultants than their predecessors. Figures obtained by Pulse under the Freedom of Information Act from 141 CCGs across England last year showed an accumulated spend of £5.66m since April on firms such as McKinsey & Company, PwC and KPMG – an average of £42,300 per CCG. Extrapolated across all 212 CCGs, this suggests just under £9m had been spent across England – just a third of the estimated £26m spent by PCTs between April and December 2012.
Reflections on the first year of GP commissioning

‘We are trying our best to get GPs involved, running monthly “time to learn” groups and in the form of monthly membership forums, and most of the GPs do come. There has been a bit of initiative that wasn’t there before. [But] there is no freedom for the CCG. It is still centrally driven’
Dr Krishna Chaturvedi, Southend CCG

‘While I respect immensely my colleagues’ amazing work at CCGs, I think [the reforms have been] a massive distraction and we’ll end up where we should have been – except with all the complicated legal framework that may need to be unpicked’
Professor Clare Gerada, NHS England’s London region clinical chair for primary care transformation

‘For GPs to think [CCGs] are making a difference, it might take a little longer. In the good ones it is beginning to happen and I think the next year will probably test that they won’t be interfered with. They have another year, maybe two, to prove themselves’
Dr Brian Balmer, chief executive of Essex LMCs
The year ahead
The next 12 months may determine the long-term future of CCGs. With ever- tightening budgets, GP commissioners are likely to have to cope with increasingly vocal warnings about crises in A&E departments, nursing and general practice.
They will have to deal with the ongoing QIPP challenge, which compelled PCTs, and now CCGs, to find £20bn worth of savings within the NHS between 2011/12 and 2014/2015.
There is also a new chief executive at NHS England to contend with – Simon Stevens, a former adviser to Tony Blair and executive vice-president of UnitedHealth Group, the largest health provider in the US. He will be charged with implementing the results of the massive NHS England ‘Call to Action’ consultation on the future of the health service, and no doubt will have a few ideas of his own on how to improve the NHS as well.
Perhaps even more important for GPs is the inevitable march towards CCGs co-commissioning primary care with NHS England, giving them greater control over the GP contract, premises and performance management. A review led by NHS England’s national director for commissioning development, Ros Roughton, is set to recommend different contractual models that would support this. However it will meet opposition from the BMA, which argues that CCGs commissioning primary care involves too many conflicts of interest.
And looking even further ahead, the general election in May 2015 could prove decisive. The Labour Party promises yet more change if it gets into power.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












