YES
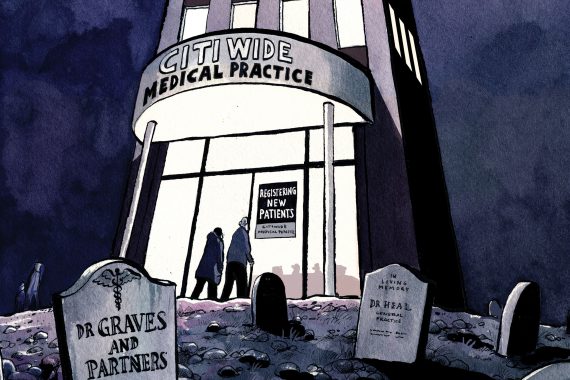
In times of plenty, small independent GP practices represent a viable business model: locally owned, locally managed and serving local needs. However, in times of challenge, it’s a different picture. Contractual and payment changes that are already in the pipeline will hit GPs hard, making it very difficult to survive, let alone thrive, as a smaller practice.
But we have opportunities to build new, different, more resilient models of primary care, to redesign, rebuild and re-establish primary care as the force for good that we all know it to be.
There are various models of ‘primary care at scale’ currently being explored. We at Lakeside Healthcare eschewed the federation model, on the basis of its being too loose in design, in favour of forming a single super-practice, with 60 partners. Our super-practice has a single operating model, a single HR model, a single IT system and crucially a single financial model. By streamlining these support functions over multiple sites, we reduce the overall unit cost and introduce the convenience for patients of being seen at one of several sites. As a sizeable counterparty, a super-practice is much more attractive to banks, so our ability to secure funding at optimal rates helps development plans.
To enjoy a devolved budget from CCGs to manage the care of patients on GP lists directly, NHS England has suggested a minimum list size of 30,000 to 50,000 patients as for ‘multispecialty community provider’. The bigger the list, the more financial resources are at the disposal of the practice.
Being bigger also allows practices to employ more specialists, both clinical (pharmacists, nurse practitioners) and non-clinical (accountants), as this cost is spread over a greater denominator. And they can attract these staff more effectively; a super-practice can offer doctors and nurses a financially attractive career with a sustainable employer.
Increasingly, patients want more from their GPs in the way of services. A small practice will struggle to have the necessary clinical skills in house to design and deliver a fuller range of services, but a larger practice can offer these specialist skills.
The size of a super-practice means it can improve its operational resilience (based on the numbers employed) and improve its financial resilience (based on the variety of contracts and income streams). This allows it to improve the range of community-based services offered to patients.
Professor Robert Harris is a partner at Lakeside Surgeries, Northamptonshire, and CEO of Lakeside Healthcare Group

NO
Under the pressure of ever-increasing demand, it is easy to understand why worn-down, burnt-out GPs look up wearily from their desks, and say: ‘A super-practice? That sounds good.’
Joining forces, whether as a super-practice, a federation or simply via an agreement to collaborate, is the ‘new black’, but this is based on a set of assumptions it is important to debunk. For instance, will recruiting and retaining those missing 5,000 GPs somehow become easy for a larger entity? Super-practices offer ‘a varied and exciting career’, according to those that run them. But any GP can easily recognise the recruitment adverts for these super-practices. Peppered with blue-sky buzzword bingo, it is not clear that these jobs are anything different from those offered by big companies a few years ago. Will there be any fewer empty chairs because practices have got together, signed a big fat legal agreement and appointed an executive board?
Partnership has been attractive in the past because it offered GPs the chance to make decisions and to have influence over how they care for patients and how they run their practices. The predictors of job satisfaction (autonomy and control, variety, social support) are worryingly absent from the big practice model – decisions are taken at board meetings to which non-executive GPs are never invited and their opinion is not sought. The ordinary GP is there to do the clinical work, to process the non-stop conveyor belt of patients.
Sitting in an identikit room, ticking boxes on management-created pop-up windows, for whatever LES or quality scheme they’ve signed up to, GP partners will wonder what benefit merging into a super-practice has brought them, other than avoiding bankruptcy. Faced with annihilation, singlehanded or small practices have gladly agreed to the loss of autonomy to survive. But the staff, who were providing a personalised service characterised by unmeasurably valuable continuity, are less enthusiastic, complaining that everything has changed, no one listens to them and its it’s all about money and targets.
I know it’s hard; I know in many practices partnership is now an impossible job. But your fear of personal bankruptcy or loss of earnings is playing into the hands of those private providers waiting in the wings. It’s not just about money, it’s about the very core of what general practice is. You are not an industrial cog in a huge machine, but if you sign up to a super-practice you might well become one.
Dr Zoë Neill is a portfolio GP in Leeds
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens