Dr Kari Nightingale and Dr Simon Tricker describe how they dramatically reduced the amount of time GPs spend dealing with correspondence
The problem
The practice is in a semi-rural town in Hampshire, with 19,000 registered patients and nine GPs across two sites. Most correspondence used to be scanned into Docman, the practice’s document management software, and sent to GPs regardless of its content. These letters sometimes took second place to urgent clinical matters, leading to delays dealing with actionable items in letters that were for information only. The surgery had received a complaint from a patient who felt their medication changes had been delayed. We decided to test whether staff other than GPs could safely deal with some of this correspondence.
What we did
The idea came from a discussion about ideas for Dr Nightingale’s forthcoming primary care fellowship, which highlighted frustration about the volume of incoming correspondence. A team was established to drive the project. This consisted of the GP fellow, the practice manager, a GP partner and an IT and data quality administrator (IDQA).
For an initial six-week period, GPs commented on a random selection of the mail items they received, completing a form describing the type of item, whether they needed to see it and why. From this we created a protocol (see above). This was further amended as the forms were analysed by the fellow. Non-clinical staff were then asked to send GPs only those items deemed necessary by the protocol, and send other items to the IDQA.
The IDQA then reviewed these items to determine whether they could be filed with no action, whether they required action, or whether a GP needed sight of them. Our IDQA has more than five years’ experience in the practice and is familiar with medical correspondence, through summarising patient notes, dealing with repeat prescription requests and identifying and inputting Read codes. He has also undertaken coding courses. Any items thought to be incorrectly directed to the IDQA were documented on another feedback form and items the GPs felt had been sent to them unnecessarily were flagged to help tailor the protocol further.
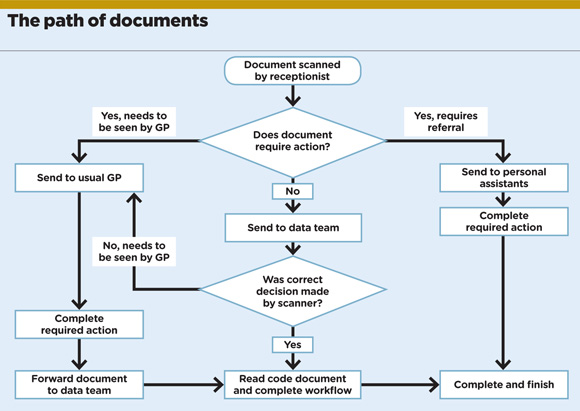
Examples of items that no longer go to GPs include referral letters sent between disciplines, notifications of completion of a course of treatment, such as physio or hearing aid fitting, letters where a patient has been discharged from a clinic, or those that state the specialty will order investigations and see the patient with results.
Items that go to GPs include those requiring action or medication changes, personal replies to letters of advice, results of investigations and letters about child or oncology patients.
Challenges
The introduction of the system started two years ago and it took around two months to tailor the protocol.
The project required willingness to change and a few hours to discuss how to start. There was no financial investment and GPs spent around one hour a week on the feedback forms until the protocol was finished. The system has continued to run successfully, and the GP partner and IDQA meet regularly to audit the IDQA’s work. The IDQA spends two to three hours daily reviewing mail items.
Results
It varies each month, but roughly 60% of all correspondence does not need to go to a GP. In July 2017, we scanned 4,393 documents, 67% of which were dealt with by the reception and triage team, and 33% of which were seen by a GP.
The GPs have loved the system, commenting that they are ‘able to keep on top of the work so letters are responded to quickly and new treatment or changes in treatment are actioned’.
The future
If you haven’t already done this in your practice, go for it.
Each practice will have its own individual preferences for what items of mail the GPs will want to see, so it is important for the system you develop to reflect this.
Our reliable IDQA has been essential in this project. If your practice has less experienced staff, you may need to adopt a more rigid protocol and have a lower threshold for items being sent to GPs.
Dr Kari Nightingale is a salaried GP at West End Surgery, Southampton and former GP fellow at University Hospital, Southampton, and Dr Simon Tricker is a GP partner at the Abbeywell Surgery in Romsey, Hampshire

















